Introduction to the Cardiac Catheterization Procedure
This article explains what happens during a cardiac catheterization and about the risks of having a cardiac cath. We tell you should do before and after this test procedure.
A cardiac catheterization is not surgery. It is a test in which a catheter (a long, thin plastic tube) is put into a blood vessel (an artery or vein) in the arm or leg and passed into the heart to get information about the functions of the heart or blood vessels around the heart in people of all ages, from newborns to the elderly. The test lasts about an hour and you don’t have to be put to sleep (general anesthesia).
This procedure gives current information about your heart and blood vessels that other tests, such as a stress test, cannot find. Knowing more about this test ahead of time may help you feel less nervous and more prepared.
Purpose of a Cardiac Catheterization
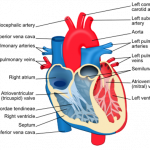
There are many purposes of a cardiac cath; some involve a procedure called angiography. Angiography is when moving xrays (angiograms) are taken of the heart and blood vessels after dye is put into the body. In general, this test is done to see if there are problems or diseases in the main blood vessels (aorta or pulmonary artery), valves or chambers of the heart, or to see if there is build up of fat in the arteries of the heart (atherosclerosis).
A cardiac cath and angiography helps:
- To find hereditary or congenital problems
- To help identify candidates for bypass surgery or cardiac stent and angioplasty
- To offer a “road map” of the coronary arteries
- To measure pressures and blood gases within the heart
- To check for narrowing or leaking of the heart valves
- To evaluate those with chest pain or cardiac diseases
- To get xrays or pictures of your heart valves and blood vessels
In addition to collecting diagnostic information, a cath allows arteries to be widened with a balloon (balloon angioplasty) or the insertion of cardiac stents. Medicines can be put in the heart to dissolve blood clots more effectively.
The Heart
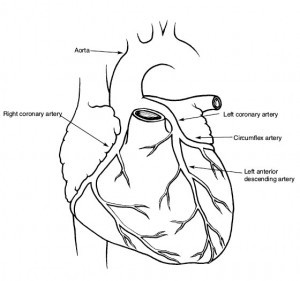
Many people think of the heart as a pump that provides the body with blood. But the heart is a muscle that has its own blood vessels to make sure that the heart gets enough blood for itself. Your heart has three main coronary artery branches, and some of them are located in the heart muscle to give the heart blood and oxygen. The left coronary artery splits into the anterior descending artery and the circumflex artery and is the primary source of blood for the left atrium. The right coronary artery supplies blood to the inferior wall of the heart. (Learn more abut anatomy terms such as anterior and posterior.)
Smoking, high blood pressure, stress, poor diet, and little exercise can damage these arteries. As a result, blood flow within the heart will decrease, and you may have a heart attack.
Warning signs of a heart attack:
- Discomfort or pressure around the chest
- Hot or cold sweating
- Aching, burning, or tightness in the upper body, back, chest, shoulder blades, arms, jaw, or neck
- Indigestion, fullness, or choking
- Dizziness or nausea
- Vomiting
- Heart beating fast
- Feeling extremely weak or having shortness of breath
Questions to About Your Cardiac Catheterization
- Which blood vessels (arm or leg) will be used for my cath?
- Who will be performing the test?
- How long will the test take?
- Where will the test take place?
- How often do you do this procedure?
- Do I have any risks?
- What should I do about medicines I take such as anticoagulants, oral hypoglycemics (diabetes medicine), medicines for erectile dysfunction (ED) and nitroglycerin?
Risks of Having a Cardiac Cath
In general, this test is considered to be very safe with little risk of problems. However, do not have this test if you have a bleeding disorder or poor kidney function. Also, the risks of the this procedure increase with:
- Stress
- Obesity
- Smoking or alcoholism
- Recent or chronic illness
- Patients older than 65
- Patients with a small body surface area
- Patients that are women
The main factors that affect the risks are the amount of experience of the cardiologists and staff doing the test and the patient’s general health and condition of heart disease. Here are other risks or possible problems that can occur:
- Excessive bleeding
- Allergic reaction to dye or anesthesia
- Infection
- Hematomas (collections of blood) where the skin was pierced to enter the blood vessel
- Blood clots in the blood vessel
- Heartbeat disturbance, rarely cardiac arrest
- Blockage of the artery causing emergency open heart surgery (rare)
- Stroke or heart attack (rare)
- Bruising where the catheter entered
- Temporary numbness at the site of the puncture
Preparing for a Cardiac Cath
Your doctor will ask you about your health history—especially about your heart—and your family’s health history, such as does heart disease run in your family. Tell your doctor and nurses about any allergies you have, such as latex, food or medicine or if you have an xray before and were allergic to the dye. You will have blood tests and an EKG; a chest xray may also be needed.
Getting Ready At Home
- Do not drink or eat anything for at least six hours before the test to reduce chances of nausea or vomiting during the test
- You may be asked to take a bath or shower the night before your cath to scrub the inside of your right arm near the elbow or both sides of your groin with soap.
- Continue taking your medicines (with only a little water) unless your doctor tells you to stop. If you take nitroglycerin, NTG, take it with you to the hospital in case you have angina.
In the Cardiac Catheterization Lab
- If this test is not being done as an urgent procedure, you may be able to come on the morning of the test instead of spending the night at the hospital the day before the scheduled test
- You may have to give information on your medical history; also know the names and dosages of your medicines
- You will be asked to sign an informed consent form (example cardiac cath consent form) giving your permission to do the test
- Tell your doctor or nurse if you are allergic to shellfish (i.e. shrimp), iodine, or the dyes that will be used during this test
- Tell your doctor if you are pregnant
- You will have blood and urine tests, an ECG (electrocardiogram, which studies the electrical activity of the heart or your heartbeat), and possibly a chest Xray
- Before the test, you should urinate. Leave behind jewelry, clothing, or anything that may interfere with the Xrays or the test itself. You may be able to wear your glasses, other jewelry and socks.
- Put on a hospital gown for the cath
- Before the catheterization, a nurse will clip or shave any hair and scrub the skin, usually the groin, where the catheter will enter through the skin and into the vein
- You may be given a sedative to help you relax
During the Cardiac Cath
Catheterization is done in a specialized, Xray equipped laboratory that is similar to an operating room. The room has an xray camera, monitors (computer screens), a table or bed, and other equipment. The team that does this test may include one or two cardiologists, an anesthetist, a nurse, and a camera operator. The team will put sterile drapes around you so that the catheters and other instruments do not touch anything that is not sterile. They will also be wearing lead aprons to protect them from the xrays. However, the xrays from this one procedure will not hurt you.

You will be lying in a bed that is under an xray camera. The bed may tilt under the camera, but in some labs, there may be an xray camera that moves over a stationary bed. If the bed tilts, you may be secured to the table or bed with straps around your waist, shoulders, and knees. You may be able to see the pictures taken of the heart and blood vessels during the test. You might also hear a beeping sound, which has to do with your heartbeat.
This test is performed as a procedure requiring a one-night stay at the hospital. Sometimes, the patient can go home on the day of the procedure; the patient has the test in the morning and goes home in the early evening. The test itself takes 1-2 hours. You’ll likely be awake (conscious sedation) during this procedure.
Medication for relaxation, sedation, and a blood thinner reaction may be given to you before the cath. A small needle will be put in a vein in your arm, and the medicine will go into the bloodstream as needed.
To begin the cath, the cardiologist uses a numbing medication (anesthetic) to numb the area where the catheter will be put in. An artery or vein in the arm or groin will be used as the site where the catheter will enter. If the doctor uses a blood vessel in the arm, a small incision will be made to find the artery or vein. As the anesthetic is injected, you may feel a slight burning or stinging sensation.
After the area is numb, an introducer sheath (tube) will be put in the artery or vein. This sheath allows the doctor to change catheters during the procedure. There should be no pain while this is being done. When the sheath is in the blood vessel, the doctor can change catheters without discomfort for you. You may feel pressure at the site of insertion, but there should be no pain. The doctor passes a catheter through the needle into the blood vessel and guides the catheter to a heart chamber or one of the coronary arteries. The catheter is a long thin tube about the diameter of a small pen refill. When the catheter is in place, the doctor can inject a contrast dye and xrays can be taken for some tests. During the injection, you may feel a hot, flushing feeling or some nausea, which will pass quickly. You may also feel your heart “skip,” but that is a normal feeling and should go away soon. You may be asked to cough or breathe deeply to reduce the nausea or light-headedness caused by the dye. Breathing deeply will allow the heart to be seen more easily.
 If there is a monitor nearby, you will be able to see the doctor guiding the catheter to your heart. The light will probably be dimmed to make the monitor screen clearer. As the catheter is in the chamber(s) of the heart, continuous xrays are taken. Also, pressure readings are made in different chambers of the heart and main blood vessels. While pressure readings are taken, you may be asked to breath, cough, stay quiet, or turn to one side. After pictures of the chamber(s) are made, the catheter is guided into the coronary artery system. Some more dye is pumped into the arteries through the catheter. Then xrays record the flow of the dye into the branches of arteries. The dye will find any narrowing or other problems in the coronary artery system. If any of the arteries are blocked, they will not fill with dye. If an artery may have spasms, the dye will usually allow the doctor to see the spasm occur. (Click on image to see dye injected into heart.) If a stent is necessary, it will be placed in the artery during the cath.
If there is a monitor nearby, you will be able to see the doctor guiding the catheter to your heart. The light will probably be dimmed to make the monitor screen clearer. As the catheter is in the chamber(s) of the heart, continuous xrays are taken. Also, pressure readings are made in different chambers of the heart and main blood vessels. While pressure readings are taken, you may be asked to breath, cough, stay quiet, or turn to one side. After pictures of the chamber(s) are made, the catheter is guided into the coronary artery system. Some more dye is pumped into the arteries through the catheter. Then xrays record the flow of the dye into the branches of arteries. The dye will find any narrowing or other problems in the coronary artery system. If any of the arteries are blocked, they will not fill with dye. If an artery may have spasms, the dye will usually allow the doctor to see the spasm occur. (Click on image to see dye injected into heart.) If a stent is necessary, it will be placed in the artery during the cath.
Recovery After a Cardiac Catheterization
When all the xray pictures have been taken and tests are complete, the catheter will be removed. Pressure is put on the area of the blood vessel that was used as the insertion site until bleeding stops (10-20 minutes). You may have stitches if an arm artery was used. Then a large pressure bandage is put on the area. You will be moved to a recovery area. A small sandbag may be placed over the insertion site to maintain pressure. You may stay in the recovery room longer if you start bleeding again or have other problems. You will need to rest in bed for about 8 hours. If the doctor used a blood vessel in the groin area as the insertion site, keep your leg straight—it doesn’t have to be stiff—for 6 to 8 hours. You can move your other leg and arms all you want. But do not sit up or turn over until a tight seal forms at the incision site. If you have to cough or sneeze, use your fingers to put firm pressure on your bandage. You can wiggle your toes or point and bend your ankle on the affected leg, just don’t bend knee or the area where the catheter was put in.
If a vessel in the arm was used, keep the arm straight for a minimum of 3 hours. Don’t bend the am sharply for several hours or lift anything heavy until the soreness is gone.
If you feel pain, a nurse can give you medicine to make you feel better. The nurse will check often to make sure that you are not having problems. Let the nurse know if you have pain in your chest, neck, or feel dizzy, weak or short of breath. The nurse will also check your bandage for any bleeding that may occur.
You may feel a little drowsy as the anesthetic from the heart cath is still working. You might feel some pain at the site where the catheter entered as the numbing starts to wear off. The dye that was used during the cath will go out of the body as extra urine.
While you’re in recovery, be sure to let the nurses know right away
- if you feel sudden pain in the area where the cath was put in,
- if you feel like your arm or leg is bleeding (wet, sticky or warm) or
- if your hand or arm hurts or feels cold.
What to Expect After Having a Cardiac Cath
You should expect complete healing without any problems. You should be able to eat and drink as soon as you would like after the cath. A hard ridge may form along the incision site, and as it heals, the ridge or bump should go away. You can also expect discoloration (bruising) where the catheter was put in; this should disappear within 2 weeks. Some people, especially the elderly and those with high blood pressure, may have a small bruise around the area where the catheter entered. The bruise will go away in a few days or weeks. Infection is rare. You may feel tired the first two days after the cath. You may also be put on aspirin and Plavix medications.
Cardiac Catheterization Results
For normal results, a cardiac cath should show no problems in the heart or coronary arteries. The arteries should have smooth and regular outlines. If your results are abnormal, the test may show coronary artery disease, disease of the heart valves, or other cardiac problems. If there are problems, the doctor will discuss types of treatments that you may need. Abnormal results may indicate a need for urgent heart surgery.
Recovery at Home
Unless you need further treatments right away you can go home after a few hours. Someone will need to drive you home. You may feel tired for a day or two after the procedure. If you have stitches, they will be removed in 6-10 days. Here are some tips on what you should do after this procedure:
- Avoid jogging, vigorous exercise, and rough activities for two weeks.
- You can walk as an exercise 48 hours after the cath.
- Do not sit for more than an hour at a time without getting up to walk around a little. to prevent clots from forming in your legs.
- Avoid any heavy lifting for a few days.
- Use a heating pad or warm compress to relieve any pain at the site of the incision.
- Shower as usual unless your doctor says otherwise. Don’t take a tub bath until the site is completely healed.
- Between showers, keep the wound dry with a bandage for the first 3 days after the procedure.
- If the site of the incision bleeds in the first 24 hours after the procedure, press a clean cloth to the site and keep the pressure on it for 10 to 15 minutes.
- Take all medicine exactly as prescribed by your doctor.
Call Your Doctor
Call your doctor if:
- You feel sudden or severe chest pain (angina)
- You have a fever over 101° F
- Pain, swelling, tenderness, redness, or bleeding increases at the incision site
- You have signs of infection (dizziness, fever, muscle aches, headaches)
- You lose sensation in the arm or leg where the blood vessel was used for the catheter
- There are new blue or purple discolorations at the site of the incision
- Your leg or arm feels weak or numb and looks pale or bluish
- The area where the needle was inserted is red, warm, or hot to the touch
- You have a pus-like discharge at the site of the incision
If signs tell you it’s an emergency or life-threatening — call 911
Summary
Cardiac catheterizations give detailed information about your heart and blood vessels that other tests cannot find. Although there are some risks, this test has its benefits. It is important to know what to expect when you’re having a heart cath. You should consider the risks involved for you when deciding whether to have a heart cath. It is also beneficial to know what happens during this procedure to help relieve your worries about the procedure. Make sure to talk to your doctor before your catheterization if you have any questions or worries.