Lung problems are not uncommon after surgery. The anesthesia medications used during surgery can affect how well our lungs work immediately after surgery. Also, inactivity after surgery (secondary to pain, drowsiness) limits amount of oxygen taken in by our lungs since we don’t breath as deeply as we do when we are active, even just doing our daily activities.
There are many kinds of surgery done under general anesthesia. With general anesthesia, you are “put to sleep” and your breathing is slowed down. The breaths you take are not as deep as you normally take when you are up and active. These shallower breaths keep some of the tiny air sacs in your lungs (called alveoli) from fully filling with air. As a result of this, these sacs can flatten. Additionally, following surgery, inactivity, pain, and the side effects of pain medications, can further contribute to this slowed, shallow breathing. This is particularly common after abdominal or chest surgery.
The collapse of these air sacs following surgery is one cause of atelectasis, which is a common minor complication seen in patients undergoing general anesthesia. Atelectasis, if more severe, can lead to hypoxia (decreased oxygenation). Atelectasis can also cause fever. If you not appropriately addressed, atelectasis can lead to complications like pneumonia or even respiratory failure.
In order to get air back into these sacs and open them up, you need to take deep breaths and hold them. Deep breathing exercises have other benefits too. They can help you to relax and assist with post-operative pain control.
If you’re in too much pain to take deep breaths, let your doctor or nurse know so that your pain can be better controlled.
Anatomy of the Lungs
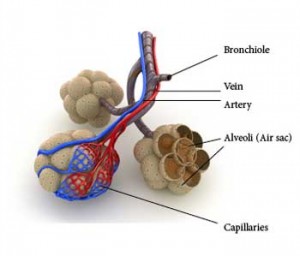 Your airway is structured like an upside down tree. When you breathe in, the air flows into the trunk-like trachea which then divides into two large branch-like bronchi. Within each lung, these bronchi further divide into progressively smaller branches. The smallest of these branches are known as the respiratory bronchioles. Attached to the respiratory bronchiole are a cluster of grape-like structures called alveoli. Alveoli are grape or balloon-like air sacs (each air sac is known as an alveolus). There are about 300 million alveoli in each lung. These tiny sacs have thin walls lines by tiny blood vessels called capillaries that allow for the exchange of gases between the air we breathe and our blood. Oxygen from the air is absorbed and carbon dioxide in our blood is breathed out by the lungs.
Your airway is structured like an upside down tree. When you breathe in, the air flows into the trunk-like trachea which then divides into two large branch-like bronchi. Within each lung, these bronchi further divide into progressively smaller branches. The smallest of these branches are known as the respiratory bronchioles. Attached to the respiratory bronchiole are a cluster of grape-like structures called alveoli. Alveoli are grape or balloon-like air sacs (each air sac is known as an alveolus). There are about 300 million alveoli in each lung. These tiny sacs have thin walls lines by tiny blood vessels called capillaries that allow for the exchange of gases between the air we breathe and our blood. Oxygen from the air is absorbed and carbon dioxide in our blood is breathed out by the lungs.
Breathing and Coughing Exercises
Practicing breathing and coughing exercises before your surgery will make it easier to do them afterwards. Again, this is particularly beneficial if you are undergoing general anesthesia. You’ll be less likely to have lung or breathing problems. If you are undergoing abdominal or chest surgery or have a history of lung problems, these exercises are even more important for your healthy recovery.
Breathing Exercises
After surgery, breathing exercises are an important part of the recovery. Doing these exercises will help prevent lung problems such as pneumonia. Breathing exercises include deep breathing and coughing. Learn and practice these exercises before surgery; practice everyday for at least a week before your surgery.
Deep Breathing (diaphragmatic breathing, abdominal breathing, belly breathing)
The chest cavity and the lungs expand when your diaphragm contracts. The diaphragm is a thin muscle located between your chest and abdominal cavities. The purpose of deep breathing is to completely fill your lungs with air. In order to accomplish this, you need to use your other chest and abdominal muscles to help your diaphragm maximally expand your chest cavity. During this type of breathing, you should feel your lungs really expand and should even feel your abdomen expanding:
1. Breathe in through your nose as deeply as you can (your stomach should go out as you breathe in). Hold your breath for 5-7 seconds.
2. Let your breath out through your mouth slowly—take twice as long to breathe out as you did to breathe in. Purse your lips (like you’re blowing out a candle) as you breathe out. Your stomach should go out as you breathe out.
Do this exercise 10 times. After you do the deep breathing exercise, do the coughing exercise.
Coughing
Coughing helps to keep your lungs clear.
1. Take a slow, deep breath in through your nose. Try to fully expand your chest and back.
2. Breathe out through your mouth; you should feel your chest sink down and in.
3. Repeat steps 1 and 2 for a second breath.
4. Take a third breath, but instead of breathing out, hold your breath for a moment and then cough hard forcing the air out of your lungs.
Do the coughing exercise 3 times. Do the combined breathing and coughing exercises every hour while you are awake.
Incentive spirometer
 Many times, after surgery, you will be given an incentive spirometer (image right) to help you to do deep breathing exercises after surgery. The hospital staff will teach you how to use it.
Many times, after surgery, you will be given an incentive spirometer (image right) to help you to do deep breathing exercises after surgery. The hospital staff will teach you how to use it.
How to use the incentive spirometer
• Sit up as straight as you can. If you’re in a hospital bed, sit on the edge of your bed or raise the head of your bed so you’re sitting up straight.
• Hold the incentive spirometer in an upright position. (see picture above)
• Put the mouthpiece in your mouth and close your lips tightly around it forming a seal.
• Breathe in slowly and as deeply as you can to raise the piston in the air cylinder up to the top of the cylinder.
• Hold your breath as long as you can (at least 5 seconds), then let the piston fall to the bottom of the air cylinder.
• Rest for a few seconds and repeat the steps above at least 10 times every hour while you’re awake.
• After each set of 10 deep breaths, do the coughing exercise described prior.
After surgery, probably one of the best things you can do for your lungs is to walk. Once you’re walking sufficiently well, you typically don’t need to continue with the breathing exercises (unless otherwise directed by your health care professional).
If You Smoke
Nicotine (which is present in any tobacco product) has been proven to interfere with both the healing and recovery processes. In order to heal your wounds after surgery, your body relies on good blood flow to get the appropriate nutrition, etc. to your wounds. Nicotine actually causes your blood vessels to constrict, which limits the blood flow to areas where it is much needed. Furthermore, smoking is independently associated with chronic lung disease, heart issues, and blood vessel issues. Smoking has been shown to raise the risk of heart attack, stroke, lung complications, and wound issues following surgery. So avoiding smoking and other tobacco products around surgery is beneficial.
Rather than have the stress of nicotine withdrawal while your body is recovering from surgery, try to quit smoking a few weeks before surgery. Talk with your surgeon before using nicotine replacement products such as a patch, gum, or cigarette substitute or to help you find ways to quit. Nicotine replacement products, contain nicotine, which again can interfere with blood flow and the healing process.
Other Considerations

Our upper body (trunk) is divided into two main cavities: the thoracic (chest) cavity and the abdominal cavity. As mentioned previously, these cavities change shape as you breathe. The chest or thoracic cavity changes volumes as you breathe (via the diaphragm.- the breathing muscle). The abdominal cavity can also change shape depending on its volume—for instance, based on how much you eat or drink. As the abdominal cavity expands, it begins to push up on the diaphragm. This is why it can be harder to breathe after a large meal. Additionally, when the abdomen pushes up on the thoracic cavity, the volume of the thoracic cavity actually gets smaller as well.
Understanding this relationship can help you understand why it is particularly painful for you to take deep breaths after abdominal surgery. When you take deep breaths, the diaphragm pushes down on the abdominal cavity, pressing on tissues “injured” during surgery causing pain. It is important to remember that this is normal. You must still continue to take deep breaths for the reasons mentioned above. Maintaining a more erect posture can give your abdomen more room to bulge and make breathing a little bit less painful.
Note that the information in this article is purely informative and should never be used in place of the advice of your treating physicians.
