A cesarean birth (cesarean or c-section) is major surgery where a baby is delivered by an incision that is first made on the skin, then the underlying abdominal muscle wall and finally the uterus itself. Cesareans can be done by an obstetrician as planned surgery or as an emergency procedure when vaginal birth isn’t possible. The American College of Obstetricians and Gynecologists recommends that non-emergency cesareans be performed no sooner than 39 full weeks of gestation. Although cesarean births are considered very safe, there are risks, including death. The reasons for and the outcome of any surgical procedure depend on age, how severe the problem is, and your overall general health.
Types of Uterine Wall Incisions
There are three types of incisions made in the uterine wall for the delivery of the baby. The type of incision chosen depends on the presentation of the baby and the speed at which the procedure can be done.
• the low vertical incision—an up-and-down incision is made in the lower, thinner part of the uterus. This incision is usually made when the baby is presenting breech—rump first or feet first.
• the high vertical (classical) incision—an up-and-down incision is made in the upper part of the uterus. This incision is made when the baby is presenting sideways or the placenta is abnormally placed.
• the low transverse incision—also called a bikini cut, is a side-to-side incision is made in the lower, thinner part of the uterus that contracts minimally during labor. This incision is made when the baby is presenting head first.
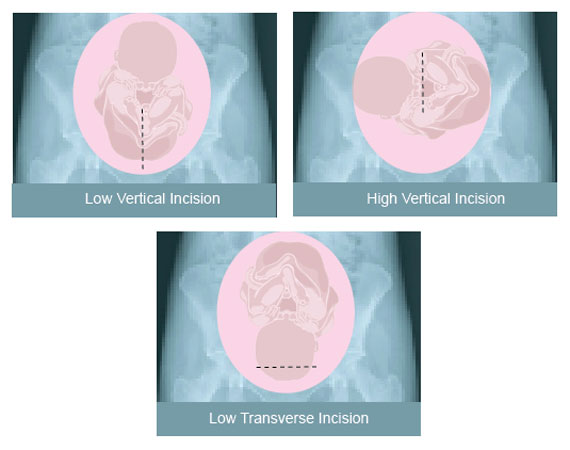
Cesareans can be done with either an up-and-down or side-to-side incision in the skin of the abdomen. Therefore, it’s not possible to know whether the uterine wall had a transverse or up-and-down incision based solely on the scar on the abdomen.
Apart from the major difference in the pattern of incision as mentioned above, there are other advantages between a low transverse, low vertical and classical cesareans:
- The chances of hemorrhage or rupture during future pregnancies in a low transverse delivery are much less compared to that of the classical delivery.
- There is less blood loss.
- The incision is easier to close up.
- There is less risk of uterine infection.
- There is a lower risk of gastrointestinal complications.
The major disadvantage to this incision is that it takes longer to do so in case of an emergency, this incision isn’t used. Today, the low transverse cesarean is preferred and performed by most OB/GYNs. The way your uterus is cut may not seem important, but it can play an important part in the decision on later births whether you can try a vaginal birth after cesarean (VBAC).

Reasons for Cesarean Birth
At one time, most babies were born by vaginal birth, which in some cases caused complications both for the mother and the newborn, which led to a high mortality rate. Cesarean births were only performed in emergency situations and most of those were the classical cesarean that had more complications. As surgical techniques and anesthesia have developed, cesarean birth has become a more common method of birth and the chances are much higher of delivering a healthy baby and reducing risks for mother.
[chart
data=”40,60″
bg=”FFFFFF”
labels=”Cesarean+Births|Vaginal+Births”
colors=”fad6e4,6b919a”
size=”425×190″
title=”Percentage of cesarean births performed each year.”
type=”pie”
]
Cesarean births are most often performed for two main reasons:
- the danger to the mother or baby would be greater with a vaginal birth
- things go unexpectedly wrong during a vaginal delivery
The following reasons fall under these two main reasons:
- Dystocia.The number one reason for cesarean birth is ‘dystocia.’ Dystocia refers to any difficulty in labor. The difficulty can be caused by:
- The fetus is not be able to progress down the birth canal. Failure of labor to progress can be caused by contractions that aren’t vigorous enough to open the cervix (dilate) enough for the baby to move through the vagina or the baby presents other than crown first that prevents progress through the birth canal. Failure to progress accounts for about 1/3 of all cesarean births.
- The size of the baby compared to the size of the mother’s pelvis—if the baby’s head is too big to pass through the mothers pelvis it can cause a very difficult vaginal delivery and even stop the cervix from completely dilating. In some cases, the pelvis may be misshapen or the baby presents the largest part of the head instead of the crown and it’s too large for the pelvis. Some babies are just too big to be born vaginally; large babies are common with gestational diabetes.
- Weak contractions in the mother’s uterus; strong contractions are needed to push the baby out from mother’s womb. Extended labor can be a risk to both the mother and the baby, more so to the baby.
- Your baby’s head is in the wrong position or presentation—the normal position at birth would be head down with the back (crown) of the head leading the way—called the cephalic presentation. This presentation makes your baby the “smallest.” If your baby presents face first or forehead first, your pelvis may not be large enough for your baby to get through.
- Obstruction or severe distortion of the birth canal (caused by pelvic tumor or fibroid tumors)
- Previous cesarean birth. There is a common saying “once a cesarean, always a cesarean.” This thinking led to an large increase in cesarean birth rates. This used to be true since most surgeons used the classical cesarean incision that had more blood loss and left weak incision sites. Weak incision sites made ruptures more common in later pregnancies. Recently, the low transverse uterine incision has become more common reducing the risk of rupture and enables a mother to try a vaginal delivery after cesarean (VBAC).
- Position of the fetuswithin the uterus. The normal position just before the delivery is a head-down (cephalic) position. If the baby presents in one of the positions listed below, vaginal delivery could lead to the trauma or death of the fetus. Sometimes the baby can be turned to allow vaginal delivery. Problems can also arise when the umbilical cord is “born” before the baby, cutting off the baby’s blood supply.
- Breech presentation. When the fetus is in a head-up, feet-first or rump-first position it’s called a breech presentation. The breech position can be further classified as frank (hips are bent and knees are straight), complete (knees and hips are bent), footling (knees and hips of one or both legs straight) or incomplete (one or both hips bent and one or both feet or knees lying below the breech).
- Shoulder. There are many shoulder presentations, however, all transverse positions (sideways) are called shoulder presentations.
- Compound. When two body parts appear at the pelvis at the same time, such as a hand beside the head, it’s called a compound presentation.
- Fetal distress is used to describe any complications with the fetus—such as abnormal heart rate from poor oxygen supply—and usually does not allow vaginal delivery. In most cases, fetal distress is lack of oxygen to the brain of the fetus (oxygen deprivation). Lack of oxygen can be caused by the umbilical cord is compressed or there are problems with the placenta, cutting off the blood supply to the fetus. Lack of oxygen can be diagnosed by monitoring the fetal heart rate. Lack of oxygen can cause very serious complications if the fetus is not delivered right away. Cesareans can also be necessary in cases of congenital (at birth) abnormalities of the fetus.
- Multiple births. When there is more than one fetus most surgeons deliver by cesarean births. Cesarean birth is a much safer method to deliver multiple babies. About half of all mothers who have twins, have a c-section, while 90% of triplets are born by c-section.
- Very premature fetus.
- Problems with the Umbilical When the umbilical cord is delivered ahead of the fetus, called cord prolapse, it causes the cord to get compressed by the baby and oxygen and the blood supply to the baby is cut off. This is an emergency that requires cesarean birth. Sometimes, the cord can be completely delivered and if the baby is coming right behind it, you may be able to have a vaginal birth. If the cord is around the baby’s neck, contractions can compress the cord causing the blood flow—and therefore oxygen—to your baby to slow down.
- Problems with the Placenta. The placenta can detach from the uterine wall (abruptio placentae) before labor begins and be life threatening for both you and your baby. Placenta previa is when the placenta partially or completely blocks the opening of the cervix. In this case, the placenta would have to be born first, leaving the fetus without oxygen. In addition, blood loss for the mother could be fatal.
- Health of the Mother.Certain health conditions of the mother can require a cesarean birth:
- History of previous problems during childbirth
- Active herpes sores
- Narrow cervix (vaginal atresia)
- Gestational diabetes
- Pregnancy-induced hypertension
- Vaginal infections or tumors
- HIV
- Cervical cancer
- Heart disease or risk of stroke
- Severe obesity
- Repeat Miscarriages: Mothers who have had repeat miscarriages in the past usually have weak uterus may need a medical procedure to stitch the cervix closed. If the stitches are in at the time of labor, the only way of delivering the baby is by cesarean.
- Rh Factor: In erythroblastosis fetalis (difference in the Rh factor of the mother and the fetus), there is a risk of fetal anemia.
- Health of the Baby. If your baby has been diagnosed with health problems, it may be better for your baby to be born by cesarean birth. Also, monitoring during labor will tell how well your baby is handling labor and how well the placenta and umbilical cord are working
Many of these complications happen in a very small number of births. And the decision for cesarean birth is decided by balancing the risks and benefits to mother and baby.
Risks to Mothers During Cesarean
Any kind of surgery involves risks, and a cesarean will, too. Risks are usually measured by the rate of deaths, complications, and disorders during or after the surgery.
Maternal deaths during cesarean birth are very rare—about 2 in 10,000. However, research shows that the death after cesarean birth is twice that of vaginal birth. This is mostly not related to the surgery, but rather illnesses or complications taking into account cesarean births are usually done for complicated pregnancies.
Like any major surgery, cesarean births have risks and possible complications:
• Endometritis. The most common complication is endometritis—the inflammation or infection of the lining of the uterus.
• Infections. Other complications include respiratory tract infection, urinary tract (bladder and kidney) infection (the second most common complications) and infection at the incision site. The risk of infection of your incision site is higher if you have type 2 diabetes, are obese or abuse alcohol. If the incision becomes infected, it increases the risk of the incision opening up.
• Reduced bowel function. Sometimes the medicines used for pain relief or anesthesia can slow down bowel functions causing gas, bloating and abdominal discomfort for a few days after surgery.
• Reaction to anesthesia. Sometimes breathing problems are associated with general anesthesia. General anesthesia is used in less than 20% of cesarean births. Also, follow your health care teams advice about ways to prevent pneumonia.
• Blood loss is higher in cesarean birth than vaginal birth, although transfusions are rarely needed.
• Accidental injury to bladder or bowel from surgery. These are rare, but can happen.
• Placenta accreta is when the placenta is too firmly or deeply attached to the uterus and can lead to hysterectomy.
Risk to Baby During Cesarean
In an elective cesarean birth performed before the mother goes into labor at full term, the infant is at risk of respiratory distress syndrome and a low birth weight if the baby’s due date is not accurate. Respiratory distress is with premature birth caused by the baby’s lungs not fully developing as they would at full term.
• Fetal injury can occur if the baby is accidentally cut or nicked during cesarean birth.
• Low Apgar scores can result from anesthesia.
Anesthesia for Cesarean
All surgery requires anesthesia since it numbs the pain. In cesarean birth, anesthesia is very important since the fetus can by affected by the anesthesia.
Three types of anesthesia used in a cesarean section:
• Spinal anesthesia – numbs your body from the chest down so you can be awake during surgery. You feel very little or no pain and very little if any medicine reaches your baby.
• Epidural anesthesia – numbs your body from the chest down so you can be awake during surgery. You feel very little or no pain and very little if any medicine reaches your baby.
• General anesthesia – makes you unconscious or “asleep.” General anesthesia is usually used in very serious or emergency cesarean births. It’s also used for mothers who don’t want spinal or epidural anesthesia
There is very little difference between spinal and epidural anesthesia. Both are administered locally—to a specific area—that numbs part of the body without putting you to sleep. Spinal anesthesia was prevalent before the popularity of lumbar epidural anesthesia that is now used for most cesareans.
The mother usually decides on the type of anesthesia after talking with her OB/GYN and anesthesiologist. Most doctors recommend local anesthesia—spinal or lumbar epidural—for an uncomplicated cesarean birth.
Cesarean Surgery

The nurses will get you ready for surgery by placing an IV in your hand or arm to give you fluids and medicines. You may also have blood drawn for blood tests. You’ll have monitors attached for watching your blood pressure, heart beat, and how much oxygen you’re getting during surgery. You’ll also have a urinary catheter inserted to drain urine from your bladder so your bladder is not in the way. Once you get to the operating room, you may have added oxygen through a mask. If you haven’t already had the epidural or spinal block, that will be done, too. If you are having an emergency cesarean you will likely have general anesthesia. If you have general anesthesia, all preparations will be done before you are given anesthesia to keep your baby from getting too much anesthetic, making it harder for him to wake up at birth. Your arms will likely be secured onto padded boards. Your abdomen will be scrubbed and drape put up below your chin to help keep the surgical area sterile. If you’re awake, you won’t be able to see what is happening. Your doctor, the anesthesiologist or a nurse will let you what is happening and answer your questions.
Once everything is ready, about a 6 inch incision will be made in the skin of your abdomen. Whether the incision is up-and-down (vertical) or side-to-side (transverse), will depend on several things—if you had a previous cesarean birth, if this cesarean is an emergency, the position of your baby or the placenta, and the size of your baby. A bikini incision is used most often for cosmetic reasons as well as it heals well and presents fewer problems in later births. If your baby needs to be born quickly, an incision just below your belly button to just above your public bone is made. This allows your doctor to get to your baby more quickly.
Once inside your abdomen, your bladder is moved to one side and a smaller incision is made in the uterus. Again, the incision in the uterus can be transverse or vertical—the type of incision made on your skin does not affect the type of incision made in the uterus. The low transverse it the most common and used in about 90% of cesareans—see illustration above. The low transverse causes fewer problems in later pregnancies because it makes a stronger scar reducing the chances of uterine rupture. In fact, you may be able to try a vaginal birth in later pregnancies.
 Your doctor presses on the top of your uterus and pulls your baby out through the incision. You won’t feel any pain but may feel some pressure or pulling because the incision is kept as small as possible. Once your baby is out, the umbilical cord will be cut—if your partner is there, they may allowed to cut the cord. Your baby will be given to the nurses to clean the airways and body. The placenta will be removed, the uterus closed with absorbable stitches, you will be closed up layer by layer. The incision on your abdomen will be closed with staples or clips. The doctor will press on your uterus to force blood and blood clots out through the vagina. You’ll be given medicine to shrink your uterus and reduce bleeding. You may also be given antibiotics to help prevent infection.
Your doctor presses on the top of your uterus and pulls your baby out through the incision. You won’t feel any pain but may feel some pressure or pulling because the incision is kept as small as possible. Once your baby is out, the umbilical cord will be cut—if your partner is there, they may allowed to cut the cord. Your baby will be given to the nurses to clean the airways and body. The placenta will be removed, the uterus closed with absorbable stitches, you will be closed up layer by layer. The incision on your abdomen will be closed with staples or clips. The doctor will press on your uterus to force blood and blood clots out through the vagina. You’ll be given medicine to shrink your uterus and reduce bleeding. You may also be given antibiotics to help prevent infection.
If your baby is OK you may be able to hold her and even nurse her, depending on the rules at your hospital. If your baby is not OK, then she will be taken to the nursery quickly for special care. The nurses with you will talk with the nursery and let you know how your baby is doing.
 After surgery you’ll be taken to the recovery room and monitored for a an hour or two. If you feel up to it, you may be able to try breastfeeding while in the recovery room. If everything is fine in the recovery room, you will be taken to your room and monitored to make sure you are OK and your uterus is shrinking. A typical stay after cesarean birth is 3 days. Most patients are encouraged to get up and move around the day after surgery. You should be able to return to normal activities in about 4-6 weeks.
After surgery you’ll be taken to the recovery room and monitored for a an hour or two. If you feel up to it, you may be able to try breastfeeding while in the recovery room. If everything is fine in the recovery room, you will be taken to your room and monitored to make sure you are OK and your uterus is shrinking. A typical stay after cesarean birth is 3 days. Most patients are encouraged to get up and move around the day after surgery. You should be able to return to normal activities in about 4-6 weeks.
Learn more about Self Care After Cesarean Birth.
Psychological Effects of Having a Cesarean Birth
When having a cesarean birth, one must consider the psychological effects. Afterward, a cesarean can be much more painful than a vaginal birth. This most often causes psychological effects on the mother and sometimes the father. Research shows that there is no effect on the newborn.
Some hospitals offer Family Centered Cesarean Births and allow the father to be present in the operating room during the cesarean birth. They also offer closer contact between the mother and her newborn after surgery and you may be able to hold your baby right after birth. If you’re having a planned cesarean, talk with your hospital about having the options they offer such as allowing your partner to cut the cord and carrying the baby to the warmer, breastfeeding in the recovery room, and allowing you to touch or hold your baby in the operating room. All of these can help you begin bonding with your newborn. If you are have an emergency cesarean, your family won’t be able to be with you.
Glossary
• Anesthesia: Relief of pain by loss of sensation.
• Breech Presentation: A situation in which a fetus would be born buttocks or feet first.
• Cervix: The lower, narrow end of the uterus, which protrudes into the vagina.
• Fetal Monitoring: A procedure in which instruments are used to check the heartbeat of the fetus and contractions of the mother’s uterus during labor.
• Placenta: Organ that provides nourishment to and takes away waste from the fetus.
• Umbilical Cord: A cord-like structure containing blood vessels that connects the fetus to the placenta.
• Uterus: A muscular organ in the female pelvis that contains and nourishes the developing fetus during pregnancy.