Your Baby
Weeks 31 to 36
This month is very important for your baby’s growth and development. Your baby weighs about 2 1/2 to 3 1/2 pounds at the beginning of the month and gains about 2 1/2 pounds during the month. Your baby grows to about 16 to 18 inches. The digestive tract and lungs are fully mature. His bones have hardened, except the bones in his skull which remain soft until after his birth. The toenails are present and the testes are descending. The skin is pink and your baby is getting more plump as he gains weight quickly. Your baby begins storing iron this month so make sure you are getting enough iron for both of you.
Babies born at 36 weeks weigh about four pounds. Their digestion and vision are well developed. They may or may not have problems breathing. Because they don’t have the body fat normally gained during the last month, they often have problems keeping their body temperature normal. Their chance of survival is about 90 percent.

As we have said, preterm labor begins when the uterus starts contracting more often than it should before the 37th week of pregnancy. Recognizing uterine contractions early isn’t always easy. Contractions aren’t always painful, and they don’t feel the same to each mother. They may even feel differently from one pregnancy to another. For some, contractions can be very intense and painful. For others, contractions can be moderate or mild, no worse than monthly menstrual cramps.
During the last half of pregnancy, it’s normal to have a few contractions. Normal contractions usually happen off and on, called irregular contractions. It’s not normal to have contractions every ten minutes or so for more than an hour. It’s important for you to recognize if, when, and how often you are having contractions. If the contractions continue and you have more than four to six per hour, your cervix can begin to open and thin out. Success in preventing preterm birth depends on preventing the cervix from opening and thinning out too much. Noticing contractions and labor as soon as they start allows treatment to begin sooner. If nothing is done and the contractions continue, preterm labor will lead to preterm birth. However, if uterine contractions are recognized early enough, preterm labor can often be treated and stopped.
- The Cervix
- The cervix is located at the bottom of the uterus. When you’re not pregnant, your cervix is long, narrow, and thick. It has a tiny opening that allows menstrual blood to flow out of the uterus. When you become pregnant, a mucous plug forms inside the long neck of the cervix
to protect your baby from infection. This plug doesn’t let anything into or out of the uterus.When the uterus begins contracting, it pulls on the cervix and causes it to change shape. It changes its shape by becoming shorter and thinner, called effacement. Effacement is measured in percentages from 0% to 100%. At 100% the cervix is as thin as paper.Contractions also cause the cervix to open or dilate. Dilation is measured in centimeters from 0 cm to 10 cm. Ten centimeters is enough for your baby’s head to get through.Changes in the cervix also help determine when you are “officially” in labor
Identifying Activities That Cause Uterine Contractions
The first step in stopping contractions is to think about what you were doing when the contractions started. Were you:
~ standing or walking for a long time such as shopping?
~ carrying something heavy such as groceries or one of your children?
~ doing strenuous housework such as scrubbing the bathtub or vacuuming?
~ doing something stressful such as arguing with a co-worker or paying bills?
Whatever you were doing, it is important that you:
~ recognize that you’re having uterine contractions
~ identify the activity that most likely caused the contractions, then stop doing that activity
~ drink one or two 8-ounce glasses of water and lie down on your left side until the contractions stop (or sit down if you can’t lie down)
Knowing which activities cause you to have contractions will help you prevent future contractions or at least cope with them better if they start again. Once your contractions stop, call your doctor and tell him you were having contractions and what you think caused them. If you start having several contractions an hour several times in one week, call your doctor.
Irritable uterus
Uterine irritability is when you have rhythmical, low intensity, contractions that last a very short time. These “wave-like” contractions can last from five to 35 seconds and studies show they can be present before preterm labor begins. You may not be able to feel these wave-like contractions. Therefore, your doctor may prescribe a uterine monitor for you to wear a few hours each day to watch and follow any activity in your uterus. Also, if you have uterine irritability, it is important to control those factors that increase the activity of your uterus. These factors may be lifting, carrying, standing for long periods, or pressure on the uterus.
Self-monitoring Contractions
 It’s often recommended that mothers at risk for preterm birth self-monitor contractions for at least one full hour each morning and again in the evening. Self-monitoring contractions means feeling your abdomen to see if you are having uterine contractions and then timing the contractions if you do. Your doctor will tell you how often to monitor your contractions. Monitoring contractions includes measuring how long they last, how far apart they are, and how many you have in an hour. Do not trust your memory or guess. If you get upset during the process, you may not be able to remember. So, have pen and paper nearby and a clock or watch with a second hand.
It’s often recommended that mothers at risk for preterm birth self-monitor contractions for at least one full hour each morning and again in the evening. Self-monitoring contractions means feeling your abdomen to see if you are having uterine contractions and then timing the contractions if you do. Your doctor will tell you how often to monitor your contractions. Monitoring contractions includes measuring how long they last, how far apart they are, and how many you have in an hour. Do not trust your memory or guess. If you get upset during the process, you may not be able to remember. So, have pen and paper nearby and a clock or watch with a second hand.
Use our Self-Monitoring Contractions Worksheet
Steps for self-monitoring contractions:
1) Empty your bladder to relieve any pressure on your uterus.
2) Drink one to two 8-ounce glasses of water; not having enough water in your body increases the level of hormones that can lead to contractions.
3) Lie down on your left side with a pillow at your back. Don’t lay on your back. It can cause contractions to happen more often.
4) Spread your fingers wide apart, then place your fingertips over the top of your uterus, up near your breastbone. Press in lightly and feel for a tightening inside your abdomen.
What does a contraction feel like?
Contractions usually begin at the top of the uterus and feel like a tightening or hardening of a muscle. Your uterus will feel harder as the tightness increases to a peak. Then the uterus relaxes or softens as the contraction ends. If you feel your abdomen tighten (contract) and get hard and then soften (relax), you’re having a contraction. You may be able to see your abdomen move as it tightens.
When the uterus contracts, it will feel hard to your fingertips – like your biceps feel when you “make a muscle.” During a contraction, your whole uterus should feel hard. So spread out your fingers so you can feel a large area. If you feel a hard “spot,” it may be your baby’s buttocks or a foot – not a contraction.
Timing contractions
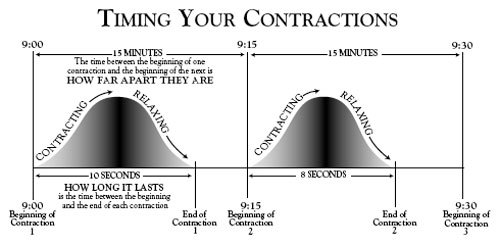
Count how many seconds each contraction lasts. When it’s over, write down the time and how many seconds the contraction lasted. If you have more than four contractions in one hour, empty your bladder again, drink at least two 8-ounce glasses of water, and monitor for a second hour. If the contractions start coming closer together or become painful, call your doctor.
How long do contractions last?
The length of a contraction is usually measured in seconds. Begin counting the seconds when the contraction begins (the uterus starts getting hard) and stop counting when the contraction stops (the uterus is soft and has completely relaxed). If you don’t have a watch with a second hand, count “one-thousand-one, one-thousand-two, one-thousand-three”. If you count to one-thousand-ten, and the contraction stops, the contraction lasted about ten seconds.
How far apart are contractions?
The time between contractions is measured in minutes. The time between the beginning of one contraction to the beginning of the next is “how far apart” your contractions are. For example, if your first contraction begins at 9:00 and the next begins at 9:15, your contractions are 15 minutes apart. If a contraction began at 9:00, 9:15, 9:30, 9:45, and 10:00, you had four contractions in one hour. The contractions are “regular” because they happened every 15 minutes.
Kick Counts
In addition to monitoring your contractions, your doctor may have you monitor kick counts. Kick counts tell how active your baby is. Besides counting kicks, you will be counting every time your baby moves or twists. Your baby has times when he is more active than others. Active times are usually after you have been up and walking around for awhile, after a meal, or after you have had something cold to eat or drink, such as ice water.
Your doctor may want you to do kick counts two or three times a day. If so, try to do them at the same time every day or after the same activity. For example, do them before you get up in the morning, an hour after eating lunch, and when you go to bed at night. If you are self-monitoring contractions, you can do kick counts at the same time.
 A good way to record kick counts is to write down the time when you start counting and the numbers 1 through 10. Every time you feel your baby move or kick, circle one of the numbers. After you circle all ten numbers, write down the time of the tenth movement. If your baby moves less than ten times in one hour, call your doctor. An easy way to monitor kick counts is with our kick counts worksheet.
A good way to record kick counts is to write down the time when you start counting and the numbers 1 through 10. Every time you feel your baby move or kick, circle one of the numbers. After you circle all ten numbers, write down the time of the tenth movement. If your baby moves less than ten times in one hour, call your doctor. An easy way to monitor kick counts is with our kick counts worksheet.
If Problems Arise or If You Go Into Preterm Labor
Before problems arise you should have a plan of action. As part of your plan, ask your doctor the following:
~ When should I call you?
~ What should I do while I wait for you to call back?
~ When should I go straight to the hospital (Under what circumstances)?
~ Which hospital should I go to?
~ Can my partner be present at delivery?
~ Who will deliver my baby?
~ Is there a chance I will have a cesarean?
~ Which hospital will my baby be in?
Signs and Symptoms of Preterm Labor
Because preterm contractions can be painless, the first symptoms of preterm labor can be easy to miss or ignore. They may not be clear or not what you expect labor to feel like, especially if this is your first pregnancy. Also, you may not be expecting any symptoms of labor at all. At 38 or 39 weeks you’re probably looking for any sign of labor and paying attention to even the slightest aches and pains. But, at 30 weeks, you may think it’s a normal part of pregnancy.
It is common to have false labor—Braxton Hicks contractions—during the final weeks of pregnancy. These contractions may be regular and painful. They usually go away within an hour or so with rest. If you have regular contractions 4 times every 20 minutes or 8 times an hour that last for more than an hour, call your doctor’s office right away.
- Labor and Contractions
- Uterine contractions supply the power that makes birth possible. Contractions are strongest
in the upper part of the uterus and push your baby downward toward the birth canal. Contractions last between 15 seconds at the beginning of labor to
90 seconds toward the end.In early labor, contractions are 15 to 30 minutes apart. Toward the very end, they are only two to three minutes apart. The first contractions are usually mild and often painless. As labor progresses they get stronger and more painful. Between contractions there is no pain at all.Uterine contractions press on the amniotic fluid and cause the bag of waters to break. As your baby’s head presses on the cervix, hormones are released that cause the contractions to become stronger and closer together. The cervix thins out and opens so your baby’s head can be pushed through the cervix and delivered from your vagina.
These are signs that can mean preterm labor is beginning.
~ Increase in uterine contractions More than four in one hour while resting, especially if they are regular (every 15 minutes) and last longer than 30 seconds.
~ Dull, low backache The backache can come and go or be constant and usually hurts below the waist.
~ Menstrual-like cramps These cramps are usually felt in the lower abdomen just above the pubic bone. They can come and go or be constant.
~ Pressure or “off and on” pains in the lower abdomen, pelvis, back, or thighs. This pressure feels like a heaviness in the pelvis “as if your baby is falling out.” It usually occurs in a regular pattern and is caused by the baby descending.
~ Fluid gushing or leaking from the vagina. This can mean the bag of waters has broken or ruptured.
~ Change in vaginal discharge in amount or appearance The amount of vaginal discharge can increase. The discharge can look like egg white or be blood-tinged, called bloody show, which can mean the cervix is opening. The discharge can also be watery, which can mean the bag of waters has ruptured and is leaking.
~ Intestinal cramping “Stomach cramps” with or without diarrhea. Diarrhea is sometimes present in the early stage of labor.
~ A “bad” feeling An “all over” feeling that something isn’t right, even if you are not sure what it is. You know your body and your baby better than anyone. Anytime you feel something “just isn’t right,” call your doctor.
Anytime you have signs of preterm labor, call your doctor right away then begin monitoring your contractions. If you are having uterine contractions and your bag of waters breaks, assume you are in labor and call your doctor right away. If your symptoms tell you it’s an emergency, such as bleeding enough to soak more than one pad in 15 minutes, call 911, especially if you are alone. Don’t try to drive yourself to the hospital.
When You Call Your Doctor
Anytime you think you are having preterm labor, call your doctor right away. If while monitoring your contractions they start coming closer and closer together, call your doctor right away.
Stay as calm as you can while you wait for him to call you back. This can be hard to do if you think your baby may be coming. So do the best you can to stay calm. Get a big glass of water to drink, then get off your feet to take pressure off your uterus. Either sit down or lie down on your left side, near the phone. Drink your water while you write down answers to the questions your doctor will likely ask.
What your doctor will want to know
When your doctor calls, he will want to find out as much as he can about your current condition and pregnancy. He may ask many questions, especially if it’s after office hours and your medical records are not available. Be sure to have your pharmacy phone number and be able to answer the following questions.
~ Are you having contractions? How far apart are they? How long do they last? How long have you timed them? Are they mild or strong? Are they regular? Do they hurt?
~ What have you tried to get the contractions to stop? (Have you been drinking water and lying down?)
~ How long will it take you to get to the doctor’s office? The hospital?
~ How many babies are you expecting?
~ How many weeks pregnant are you?
~ Has the bag of waters broken? (a gush of water or leaking)
~ Are you having any bleeding? If so, how many pads have you used?
~ Are you having diarrhea, vomiting, chills, or pain?
~ Do you have a fever? What is your temperature?
~ Do you have a cerclage (a stitch in your cervix)?
~ Have you ever had a cesarean birth?
Depending on several factors – such as how long it will take you to get to the doctor’s office or the hospital and how many weeks pregnant you are – your doctor may have you monitor your contractions for awhile longer, come into the office, or meet him at the hospital.
If Your Doctor says “Meet me at the hospital”
It’s important to have a “plan of action” in case your doctor asks you to meet him at the hospital. Your plan should include help from several people, such as friends, relatives, neighbors, and co-workers. Be sure each member of your “team” has every other member’s home, work, mobile, and pager telephone numbers. They should also have the name and telephone number of your doctor and the hospital where you plan to deliver. They should all know the shortest way to the hospital where you plan to deliver, as well as the hospital nearest to your home and your work. Most hospitals have a map that you can make copies of and give to your team members. Make several copies for yourself. Keep one at home, at work, and in the car.
At the hospital
When you arrive at the hospital, you’ll be admitted to the maternity unit. The nursing staff is specially trained to care for mothers in labor. The staff may listen to your baby’s heartbeat, check your baby’s position, measure your pulse and blood pressure. You may have a vaginal exam to see if the bag of waters has broken and check your cervix to see if it is opening. A monitor may be placed around your abdomen to record how long and how strong the contractions are and to record your baby’s heartbeat. Tests may be done and the likely cause for your early contractions will be determined. For example, you may have an infection of the cervix or urinary tract or be dehydrated.
Preterm labor is diagnosed by checking for changes in your cervix while you’re having regular contractions. Your doctor will have to examine you and may use the following tests to help determine if you are in preterm labor:
• Fetal monitoring—records the heartbeat of the fetus and contractions of your uterus.
• Ultrasonography—measures the length of the cervix and estimates the size, age, and position of your baby.
• Fetal fibronectin—measures the amount of a certain protein that helps predict the risk of preterm delivery.
• Pelvic exam and other tests to check for infections of the cervix or vagina.
If you and your baby aren’t in danger, your doctor may try to stop labor. If so, medicines are usually started quickly. An IV will be placed in your arm to give you fluids and keep you hydrated. Medicines to stop preterm labor can be given through the IV.
Sometimes labor is too far along to stop. Also, in some cases, it’s better if your baby is born right away and very likely by cesarean birth. Your doctor will decide whether it’s safer for your baby to stay in your womb and mature a little longer or to deliver your baby and give him special care. Some reasons for going ahead with preterm delivery include:
• Infection
• High blood pressure
• Bleeding
• Signs that your baby may be having problems
Medicines that prevent preterm labor
Medicines called tocolytics reduce uterine irritability and prevent or stop preterm labor. They do so by relaxing the uterus and stopping the contractions. Some tocolytics can only be given while you are in the hospital. Others can be taken at home.
Tocolytics do have side effects: they can make your heart beat harder or faster than normal and make you feel restless, dizzy, or nervous. Other side effects include headache, feeling warm, or retaining water. Tocolytics can also have some short-term effects on a baby. The usual side effects for the unborn baby are an increase in heart rate and a low blood sugar level. You’ll probably be wearing a fetal monitor so your healthcare team can watch how your baby is affected by the medicine and your contractions.
You must stay in the hospital until the contractions have stopped. It may take a few days to figure out the right dose of medicine to prevent further contractions. Once labor stops, you can begin taking tocolytics by mouth. If the bag of waters hasn’t broken and the oral dose keeps the uterus relaxed and the contractions stop completely, you may be allowed to go home. For some mothers, these trips to the hospital can happen several times before their baby is born.
Medical Care at Home
A home care program can include bed rest, taking tocolytics, and monitoring the activity of your uterus and unborn baby. Total bed rest means you are lying down on your left side and only allowed to get up to go to the bathroom. You will probably wear a belt around your abdomen that senses and records uterine contractions. The belt can send data over the telephone to a nurse. After reviewing the data, the nurse may call and talk with you or call your doctor to let him know how you are doing.
A very important part of home treatment is learning as much as you can about what may be causing your contractions and what you can do to prevent them.
Nursing care at home
If you are on total bed rest, your doctor may order home nursing care for you. Bed rest is important because it keeps pressure from you baby off your cervix. If so, a home care nurse will visit you. She will ask you how you are doing, feeling, and coping with bed rest. Talk with her about any concerns you have about your baby or problems you are having with medicine or bed rest. Your healthcare team will be happy to answer any questions you have.
During her visit, the nurse will check your blood pressure, temperature, and pulse. She may take blood or ask for a urine sample if your doctor has ordered lab tests. She may also do a vaginal exam to check for changes in your cervix. She will check your IV or pump if you have one. She can also teach you about:
~ using special equipment such as a fetal or uterine monitor, or infusion pump when she isn’t there
~ how and when to take your pulse and temperature
~ how to check for and monitor contractions twice a day
~ resources in your community
~ what tests you can expect and the risks and benefits of those tests
~ the side effects of any medicines you are taking and which side effects you should report to your doctor
Your nurse will also let you know how you and your baby are doing or if your doctor wants to modify your care, diet, or activity level.
Taking Medicines at Home
If you take oral tocolytics at home, it’s very important that you take your medicine exactly as your doctor prescribes. This includes taking your medicine at the right time and in the right amount. You may have to take medicine during the night. Keeping a clock nearby can help remind you to take your medicine. Also, it can be helpful to set an alarm or keep a daily diary to track your medicine. Don’t put off taking your medicine. It’s important to keep a certain amount of medicine in your system at all times. If you miss a dose of medicine, take it as soon as you can. Then watch for contractions. Don’t stop taking your medicine unless your doctor says it’s okay.
Because tocolytics can cause rapid heart beats, your doctor may have you take your pulse before you take each dose of your medicine. To take your pulse, place two fingertips on the palm side of your wrist, about an inch below your thumb. Feel for your heart beat (pulse). Count the number of heart beats in one minute. If your pulse is above 120, call your doctor before taking your medicine.
If the oral dose of tocolytic doesn’t prevent contractions, your medicine may be given as shots, an IV, or with an infusion pump inserted just under the skin. The infusion pump has a timer and a measuring device that gives the right dose of medicine at the right time.