Total or partial joint replacement with a prosthetic joint has become a more common treatment to relieve pain and restore independence. Most joint replacements are done for hips and knees, but shoulder replacement is becoming more and more popular as a remedy for arthritis and fractures of the shoulder. Shoulder replacement is recommended to repair painful arthritic shoulders and increase limited motion. Replacement involves the replacement of just the head of the humerus (hemiarthroplasty) or the entire shoulder joint (total shoulder arthroplasty).
More recently, the reverse total shoulder arthroplasty has emerged as an excellent surgical option in patients who are not candidates for a total shoulder arthroplasty.
The Shoulder Joint
There are two bones that form the glenohumeral (GH) joint, the main joint of the shoulder: the scapula (shoulder blade) and the humerus. The GH joint is a ball-and-socket joint, similar to the hip joint. It is the most mobile joint in the body.
The glenoid is the shallow, recessed, portion of the scapula that forms the socket of the GH joint. The humerus has a ball-shaped head which fits into the glenoid socket to form the GH joint. The head of the humerus (ball) and the glenoid (socket) are both covered in slick hyaline (or articular) cartilage, which allows smooth and pain-free shoulder motion. The GH joint is stabilized by strong ligaments and muscles. The main groups of muscles that acts to stabilize the GH joint are the rotator cuff muscles.
See Shoulder Structure, Function for more information about shoulder anatomy.
Causes for Shoulder Joint Replacement
Shoulder replacement may be a surgical option when there is severe destruction of the GH joint from osteoarthritis, rheumatoid arthritis, osteonecrosis (bone death), or trauma. Ultimately, if any of these conditions results in a painful and dysfunctional shoulder that makes it difficult to dress and care for oneself, shoulder replacement may be a good treatment option. It is important to remember that shoulder replacement is an elective surgery in most situations. This means, that most commonly, you decide when it is time to have your shoulder replaced.
The most common reason to undergo shoulder joint replacement is osteoarthritis. To make things simple, osteoarthritis is the wear and tear-type arthritis. The slick articular cartilage that covers both joint surfaces (the ball and the socket) that allows for smooth and pain-free motion ultimately wears down with time. In end-stage osteoarthritis, all of the cartilage is gone, causing bone to rub on bone. This may lead to a very painful and poorly functioning shoulder.
While osteoarthritis is more common in the weight-bearing hip and knee joints, it also commonly affects the shoulder joint. Trauma, like fractures or dislocations of the shoulder, can unfortunately accelerate this process.
Rheumatoid arthritis, which is an inflammatory type arthritis, can also result in progressive destruction of the shoulder joint leading to pain and poor shoulder function.
Osteonecrosis (bone death) of the humeral head can also result in a very painful and dysfunctional shoulder. Osteonecrosis is a condition where the blood supply to a particular bone is cut-off. Eventually this causes the bone to die. In the shoulder, osteonecrosis can occur for numerous reasons including fracture and steroid use. People with various blood diseases like Sickle Cell disease are also at risk.
Sometimes, a surgeon may recommend shoulder replacement with severe fractures of the humeral head. Severe cases of rotator cuff tears, particularly if accompanied by severe arthritis, may also be treated with a special type of shoulder replacement called a reverse total shoulder arthroplasty.
Surgical Options for Shoulder Replacement
Replacing or reshaping the damaged or diseased joint with a prosthetic one is called an arthroplasty. Depending on your age, overall health, and your specific shoulder joint problem, your surgeon may recommend one of the following procedures:
• partial shoulder replacement (hemiarthroplasty)
• partial shoulder resurfacing
• reverse total shoulder replacement
• total shoulder replacement
Hemiarthroplasty replaces the head of the humerus with a prosthesis. The glenoid surface is left alone. Hemiarthroplasty can be done to repair a fracture of the humeral head or neck when the glenoid cavity isn’t affected and is still functional. Besides fractures, other indications for hemiarthroplasty include:
• osteoarthritis
• osteonecrosis of the humeral head
• Tumors of the humeral head
• Rotator cuff tears that can’t be repaired, especially if accompanied by severe arthritis
Shoulder resurfacing replaces the surface of the humeral head with a metal covering, or cap. The glenoid surface may also be replaced using a plastic prosthesis. Shoulder resurfacing may be an option for younger, active patients with:
• osteoarthritis
• osteonecrosis of the humeral head
• Rotator cuff tears that can’t be repaired, especially if accompanied by arthritis
A major advantage of resurfacing is that it preserves bone for future shoulder procedures and surgeries. However, resurfacing is not recommended when severe bone loss is present or if the bone is not healthy enough to support the prosthesis.
Total shoulder arthroplasty replaces both the humeral head (ball) and glenoid (socket) with a prostheses. Usually the ball is metal and the socket is made of plastic. Total shoulder replacement is used when there is severe destruction of both the humeral head and glenoid surface from osteoarthritis, rheumatoid arthritis, osteonecrosis, or trauma.
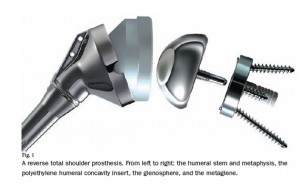 Reverse total shoulder replacement converts the head of the humerus from its normal ball structure to a socket and the normal glenoid socket into a ball. Ergo, reverse total shoulder arthroplasty. This change in the normal anatomical relationship allows us to use the deltoid muscle to compensate for the loss of function of the rotator cuff. Therefore, the main indication for this surgery is pain, and functional loss due to a severe rotator cuff tear that cannot be repaired (irreparable). Oftentimes, this leads to significant arthritis known as cuff tear arthropathy. Additionally, the reverse total shoulder replacement is sometimes used for the treatment of severe fractures of the humeral head and neck.
Reverse total shoulder replacement converts the head of the humerus from its normal ball structure to a socket and the normal glenoid socket into a ball. Ergo, reverse total shoulder arthroplasty. This change in the normal anatomical relationship allows us to use the deltoid muscle to compensate for the loss of function of the rotator cuff. Therefore, the main indication for this surgery is pain, and functional loss due to a severe rotator cuff tear that cannot be repaired (irreparable). Oftentimes, this leads to significant arthritis known as cuff tear arthropathy. Additionally, the reverse total shoulder replacement is sometimes used for the treatment of severe fractures of the humeral head and neck.
To be a good candidate for this surgery, you must have a functional deltoid muscle and a lifestyle that will put a low demand on your shoulder. Although reverse shoulder replacement is relatively new, it has emerged as a successful treatment for patients in the right situation.
Getting Ready for Shoulder Surgery
The decision of going ahead with shoulder replacement surgery should be made together with your surgeon after you have undergone a thorough orthopedic evaluation. The surgeon will tell you the alternatives of having surgery, the benefits of having shoulder replacement surgery, and the risks involved so that you can make an informed decision. If you have any questions or concerns, you should get them cleared up before signing the informed consent form. By signing the consent form, you are saying you know why you are having the surgery and that you understand the risks, benefits and alternatives of surgery and agree to the procedure.
Its important to remember that in most situations, shoulder replacement surgery is not an emergency. There are many non-surgical options that should be tried first prior to deciding to proceed with surgery. Be sure to work with your surgeon to discuss these options.
Risks of Shoulder Replacement
The risks of having complications vary from person to person. That’s because each persons health status is different. Complications differ as well, depending on the type of shoulder replacement being performed. While generally speaking, complications are uncommon, they are nonetheless, real risks that need to be heavily considered before deciding to proceed with surgery. Problems that can occur after shoulder replacement include:
• Infection (most susceptible within the first two years)
• Instability of the glenohumeral joint
• Dislocation – most likely to occur during the healing process, which is why it’s important to wear the shoulder immobilizer
• Stiffness in the shoulder – following your physical therapy routine can help prevent stiffness
• Component failure or loosening, which will lead to additional surgery
• Incomplete pain relief
• Rotator cuff tears
• Fractures of the humerus or glenoid
• Deep vein thrombosis
• Pneumonia
• Nerve injury
As with all surgery, there are also risks associated with undergoing general anesthesia, including heart attack, stroke, and even death.
Pre-op Tests and Preparation
If you decide to proceed with surgery, depending on your age and overall health, your surgeon will likely have you see your primary care physician for a pre-operative work-up. If you have known heart conditions, this may also include a visit to your cardiologist. Your surgeon may also order tests such as:
• urinalysis
• chest x-ray
• EKG
• Blood tests (depending on your medical history)
These tests are to make sure that you are healthy enough to have surgery and to prevent possible complications during and after surgery.
If you are taking certain medicines like aspirin, ibuprofen, or other anti-inflammatory or arthritis medications, you may be asked to stop taking these a week or two prior to surgery. These medications can thin the blood and cause excessive bleeding during surgery. Also, be sure to tell your surgeon about any other medicines that you take so that he can advise whether to stop taking them. Also, if you get a cold, flu, cough, or infection prior to your surgery date, let you surgeon know because your surgery may have to be postponed.
If you are a smoker, you should quit smoking as far prior to surgery as possible, as smoking can cause complications during the surgery and slow down healing.
Your surgeon may also have you visit the physical therapist that will be taking care of your rehabilitation after surgery. The therapist will be able to prepare you for the surgery and get to know your physical condition before the surgery. This will make it easier for the therapist to offer the best treatment and therapy exercises for you after surgery.
Getting Your Home Ready for Your Return
Arrange your home for your return before you go for surgery. You will need some help after the surgery as you won’t be able to move your shoulder or arm. Arrange for a family member or friend to be with you all the time for at least the first week after surgery. You also need to arrange for transportation to and from the hospital for surgery as well as for follow-up visits after surgery, since you will not be able to drive for six weeks or longer.
You may not be allowed to take a shower for a few days following surgery, so you’ll need help with a sponge bath. You also want to prevent falls of any kind, especially in the shower. Putting up temporary handrails in the shower will help you step safely in and out.
Your arm will likely be in an immobilizer sling and you may not be able allowed to do much with your arm after surgery. Go through your home and make sure that any items you will need access to are placed at waist level so you can get to them easily.
Going for Shoulder Surgery
Usually, on the day of the surgery, you will be admitted to the hospital or surgical unit early in the morning. The night before surgery, you must not eat or drink anything after midnight. Bring anything to the hospital your surgeon has asked you to bring including medications that you are currently taking as you may be in the hospital for a day or two. Take a shower and wash your hair before admission—it will be hard to wash your hair after surgery because you can’t raise your arm. Try to get to bed early and get a good night’s sleep.
Shoulder Surgery
On the day of surgery, you will be asked to arrive a couple of hours prior to surgery. If you have not already met with the anesthesiologist, the anesthesiologist will evaluate you before surgery. Usually, in total shoulder replacement surgery, regional anesthesia is used. This consists of a nerve block, where the shoulder region and arm are made to feel numb. This can last for up to a 1/2 day after surgery.
The surgery itself takes about 1 – 2 hours, however, the whole surgical process can take up to 6 hours (getting put to sleep, waking up, etc.). When the procedure is complete, the typical 4-6 inch surgical incision is closed with either stitches or staples, covered with a bandage, and your arm is usually immobilized with a sling.
In the Recovery Room
After surgery, you will be taken to the recovery room where you are monitored until you wake up and/or the effects of the anesthesia wear off. This usually takes about 1-2 hours.
To help prevent blood clots in the legs, you will likely be wearing compression stockings and a sequential compression device. You may also be given anticoagulation medicine. To further prevent blood clots, you need to get up and walk around soon after surgery. Your arm will be in a sling and may affect your balance, so be careful when you first try to walk.
From recovery you will be taken to your hospital room where you will stay for usually one to two days depending on your progress. You’ll be asked to breathe deeply and cough frequently in order to relieve any lung congestion from surgery.
Pain control is very important after surgery. Controlling pain allows you to take deep breaths, get up, move around, and participate in physical therapy—all of which decreases complications from surgery. Pain medications will likely consist of both intravenous (injectable) and oral medications. Talk to your surgical team beforehand about any concerns regarding pain control.
A special cooling machine made to fit the shoulder may be used to help and relieve pain and swelling of the shoulder area. This is usually started in the recovery room and typically costs extra. Your surgeon may send you home with the ice machine or have you use ice packs to control pain and swelling.
It may take up to a 1/2 day to regain total feeling in the affected shoulder and arm if you received a regional block. Once your regional anesthesia wears off, move your fingers and make a fist off and on to help to maintain the blood flow to the area and speed healing.
Sometimes, the surgical team will places a drain in your shoulder during surgery. If they have, it is usually removed the day after surgery unless there is still a lot of drainage.
More recently, same-day (outpatient) surgery is being done at some centers for shoulder replacement surgery based on health status. If you had same-day surgery, you will be allowed to go home when the effects of anesthesia have worn off, you’re past the stage where complications are likely to occur and you’re pain is reasonably controlled. A nurse usually reviews home-instructions with you, helps you get your prescriptions, and tells you when to make a follow-up appointment with your surgeon. He/she will also instruct you on what to do if you have problems when you get home.
The stitches inside your shoulder (under the skin) will dissolve, stitches or clips in the skin will be removed 10-14 days after surgery. Keep the incision dry until it is well healed.
Recovery and Home Care After Shoulder Surgery
Wearing a Sling
You will likely be wearing a special sling that immobilizes the shoulder when you come out of surgery. The sling has a strap that goes around your waist. Your elbow should fit far back into the sling; the sling should support and cover your wrist and hand up to your knuckles. Your fingers should be exposed so you can use them. The sling provides support, decreases swelling, and increases comfort while your shoulder heals. Your surgeon will tell you how and how long to wear the sling—usually 4-6 weeks. You will be shown how to take the sling on and off so that you don’t injure your shoulder. Do not remove your sling except to dress, shower, and do your physical therapy exercises. For the first 6 weeks, all activities of daily living should be done using your “good” arm.
You must wear the sling even in bed. It’s best if you lie on the opposite side or your back. Use pillows to help you get comfortable and keep you from rolling onto your affected shoulder during the night. Do not lie on your affected side for the first 6 weeks, or until your surgeon says it’s OK. Some people find it easier to sleep in a recliner with pillows to support their arms.
Weight Bearing Activities While Healing From Shoulder Surgery
You will likely have limits on the activities you can do with your shoulder (depending on the surgery that was performed). Some of these include:
• do not pull objects toward your body
• do no roll your shoulder backward
• do not take your elbow behind the body
• avoid putting weight on the affected arm
• do not use the affected arm to push up from a sitting position
• do not use the affected arm to lift objects
• do not use the affected arm until your surgeon says it’s OK
It is very important that you fully understand your individual restrictions. Take extra time to review these with your physical therapist and surgical team while in the hospital.
You may be allowed to shower 72 hours after surgery if you cover the surgical incision and dressing with plastic wrap. If you’re not to take a shower, take a sponge bath until after the staples or sutures are removed (usually 10 to 14 days after surgery) and the incision can get wet. Don’t bathe in tub or soak in a pool or hot tub where the incision is under water for at least 1 month. Again, review these instructions with your surgical team.
Physical Therapy in the Hospital
A physical therapist will likely work with you in the hospital and teach you the proper way to do exercises that you will continue once you get home. Make sure you carefully follow the home exercises the physical therapist gives you. Do not overdo the exercises even if you feel like you can. Do your exercises exactly as prescribed. Ask, ask, ask, if anything is unclear to you. Improper use of the joint while it is healing can lead to permanent problems or need for additional surgery.
When to Call Your Surgeon
Shoulder replacement is usually a very successful operation, but like any other surgery, there are associated complications as listed above. Call your surgeon immediately or go to the nearest emergency department if you experience any of the following once you get home:
- If you are having chest pain or difficulty breathing.
- If your arm, thigh, or calf, begins to swell or becomes increasingly painful
- If you notice any discoloration of the arm
- If you notice any progressive numbness of the affected arm after the regional block has worn off, or if the block never wears off
- If pain in your shoulder gets worse or uncontrollable despite proper use of medication
- Any fevers higher than 101.5°F
- If you experience any excessive nausea or vomiting
- If you experience continued draining or bleeding from the surgical incision
- If any signs of infection around the surgical incision: redness, swelling, hotness to touch, pus-like drainage
Keep 24-hour phone numbers handy. Call your surgeon’s office if you feel you are not healing as you should. Check your incision every day when you change the bandage for signs of infection and to make sure it is healing as it should. If you think you have a fever take your temperature. If you have signs of infection or other complications, call your surgeon right away.
It is important to remember that with any joint replacement surgery, continued drainage is a big problem and a significant risk factor for infection! Let your surgeon know right away if your wound is continuing to drain.
If the signs tell you it’s an emergency and you cannot reach your surgeon, call 911.
Physical Therapy Program After Shoulder Replacement
Restoring movement to the shoulder and arm is a very critical factor in recovering from shoulder replacement surgery. Soon after the surgery, the surgeon or physical therapist will teach you exercises that will prevent your wrist, elbow or shoulder from becoming stiff, which will speed up your recovery. Make sure you understand the expectations regarding physical therapy following surgery.
When you begin your first therapy sessions, pain may make it difficult for you to do the exercises. Slowly, it will get easier each day. Initially, expect to need some pain medications before and after therapy to help with the pain.
See Shoulder Rehab to learn more about rehab exercises for the shoulder.
Long-term Care for Your New Shoulder
Most importantly, keep your follow-up visits with your surgeon and perform your therapy exercises as advised. It will take time for you to get back to your normal activities. Depending on the type work you do and the type of surgery performed, you may be able to return to work in 8 weeks. If you have a physical job, it may be much longer. Do not drive until your surgeon says it’s OK.
The fastest way to achieve total recovery long-term is to stay active by walking, dancing, doing yard work, and, if OK with your surgeon, playing golf or swimming. These exercises will increase your strength, flexibility, and build endurance. It is important to discuss with your surgeon if there are any restrictions on how much weight you can lift and what activities you should avoid long-term. Oftentimes, these long-term restrictions differ depending on the type of surgery you had.
It is possible that your surgeon may have you take antibiotics before any future invasive medical or dental procedure in order to decrease the risk of infection in your shoulder. Make sure you have this discussion with your surgeon.
Traditionally, shoulder replacements have a life expectancy of 10-20 years depending on how active you are with your new joint. Being very active puts added demands on your new joint and may reduce the life of that joint.
Recovery Timetable (can be variable):
- 3 months after surgery: most patients are reasonably comfortable; have motion of about half of normal, but notice they have some weakness.
- 6 months after surgery: most patients are pain-free (although weather has some effect); they have motion and strength of about two-thirds of normal.
- One year after surgery: about 95% of patients will be pain-free, and the remaining 5% will usually have no more than a weather ache or an occasional ache with overactivity. There probably won’t be significant strength limitations depending on the condition of the rotator cuff and deltoid muscle.
Note that the information in this article is purely informative and should not be used in place of recommendations from your surgical team.
