What is Osteoarthritis?
Prior to reading this article, it will be helpful to review normal knee anatomy and function.
There are more than an estimated 50 million Americans who are affected by doctor-diagnosed arthritis. This number is expected to reach 80 million by the year 2040. Fortunately, about half of people with arthritis do not have symptoms. That being said, arthritis is the leading cause of disability in the United States. There are many causes of arthritis. It can be secondary to wear and tear and genetics (osteoarthritis), trauma (traumatic arthritis), inflammatory diseases (such as rheumatoid arthritis, gout, psoriasis, etc.) The most common form of arthritis is osteoarthritis.
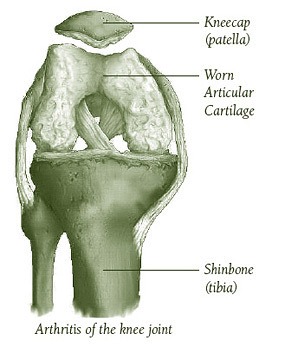 Osteoarthritis is also called degenerative arthritis, or wear-and-tear arthritis. Just like treads on a tire wear out with use, so does the cartilage on the ends of the bones within all joints of the body, wear down with time and use. Therefore, osteoarthritis is a present in many individuals by the time they reach middle age.
Osteoarthritis is also called degenerative arthritis, or wear-and-tear arthritis. Just like treads on a tire wear out with use, so does the cartilage on the ends of the bones within all joints of the body, wear down with time and use. Therefore, osteoarthritis is a present in many individuals by the time they reach middle age.
For example, if X-rays are taken of anybody over the age of 60, more than half of them will have evidence of arthritis in their joints — regardless of the body part. i.e. the longer you live, the more likely you are to have osteoarthritis.
Osteoarthritis in the knee can also result from an injury to the knee earlier in life. Injury to the cartilage, or a fracture of the bones involving the joint surface, ligamentous injuries, and injuries to the meniscus can accelerate the degenerative process, leading to early arthritis.
Research also shows that genetics can make someone more prone to developing osteoarthritis. Therefore, if your mother or father had osteoarthritis, you are much more likely to develop it at some point as well.
As specified earlier, the main issue in osteoarthritis is the gradual wearing away of the articular cartilage that covers the ends of the bones within a joint. This loss of cartilage protection results in areas of exposed bone. Thus once the cartilage has worn down, bone begins to rub against bone. The body typically responds to this rubbing by forming bone spurs around the joint.
As this is all happening, symptoms the individual may experience include joint discomfort, pain, stiffness, or even a sensation of grating within the joint. More advanced arthritis can sometimes even result in a deformity of the knee. Once osteoarthritis becomes symptomatic, the pain usually occurs with movement and goes away with rest. Pain can be worse at the end of the day.
Causes of Osteoarthritis in the Knee
The factors that contribute to osteoarthritis include genetics, obesity, and repetitive stress injury to the knee. Additional causes of osteoarthritis of the knee include:
• Removal of the meniscus
• Meniscal tears
• Abnormal alignment of the knee
• Chronic inflammation or infection
• Fractures of the bones that involve the joint surface
Symptoms of Osteoarthritis
Osteoarthritis typically develops slowly over many years. Osteoarthritis may not be symptomatic. However, if symptoms are present, they typically include knee pain, swelling, and knee stiffness. Pain is usually worse after activity.
As osteoarthritis progresses, the pain can begin to interfere with even simple daily activities. In the late stages of osteoarthritis, pain may be more constant. Additionally, you may even experience locking of the knee.
It is important keep in mind that there is no way of predicting who will become symptomatic, when osteoarthritis will become symptomatic, and over what time span symptoms will improve or worsen with non-surgical treatment.
How is Knee Osteoarthritis diagnosed?
The diagnosis of a knee osteoarthritis begins with your doctor asking you questions about your symptoms. Your doctor will perform an examination of your knee to give him/her clues regarding the cause of your symptoms.
The radiographic examination of choice for the evaluation of arthritis is a X-ray. X-rays of knees with severe arthritis will show narrowing of the space between the femur and tibia, the presence of bone spurs, and possibly cysts within bone as well.
How is Knee Osteoarthritis treated?
Unfortunately, there is currently no cure for osteoarthritis. Sometimes, patients with knee arthritis may not have any pain, then suddenly have flare-ups for no apparent reason.
There are two broad categories of treatments for knee osteoarthritis: non-surgical treatments and surgical treatment. Treatment of knee arthritis almost always starts with non-surgical modalities aimed at reducing your symptoms. These modalities include the following:
- Activity modification (avoiding activities that cause pain)
- Anti-inflammatory medications (acetaminophen, ibuprofen, naproxen, etc.)
- Physical therapy (to strengthen the muscles around your knee that support the joint)
- Weight loss
- Knee injections (steroid, hyaluronic acid, PRP)
- Bracing
There are various injections that are available for the treatment of pain related to osteoarthritis. A cortisone injection is a powerful anti-inflammatory which can oftentimes provide excellent symptomatic relief. However, used excessively, they can actually speed up the degeneration process. As such, these shots are typically only given every 3-4 months.
Hyaluronic acid injections (sometimes called gel or rooster comb injections) aim to restore the normal lubricant within the knee. They are typically considered a last resort prior to knee replacement surgery, as the evidence supporting their effectiveness is weak.
More recently, there has been an increased interest in the use of injectable platelet-rich plasma (PRP). Simply put, PRP consists of healing factors that are harvested from your own blood. The idea behind PRP is that it stimulates regeneration of damaged tissues. While the evidence supporting use of PRP in tendon issues (tennis elbow, achilles tendonitis) is encouraging, evidence to support its use in the setting of arthritis is inconclusive. Similar to the hyaluronic acid injections, however, they can be considered a last resort if you are trying to delay the need for knee replacement surgery.
Finally, the use of injectable stem cells has also become increasingly common. Unfortunately, the research in regards to the utility of stem cells for the treatment of knee arthritis is even less conclusive.
Whether or not these more modern injectables are an option for you is a discussion that you should have with your doctor.
Ways to Protect your Joint
Muscular control: Sometimes the knee gets an extra jolt when you accidentally miss a stair or when you stub your toe. Untrained leg muscles are slow to respond and protect the knee joint. These jolting forces can irritate the exposed bone. Conditioning exercises can train your knee muscles to generate force more quickly and act as shock absorbers to protect the knee joint.
Walking aids: While not ideal, the use of a cane or a walker can help to take some of the stress off of the knee — potentially decreasing the symptoms associated with knee arthritis.
Knee Braces: Oftentimes, one part of the knee has more severe arthritis (typically medially – inside) and an off loader brace can help to “offload” or take pressure off of this portion of the knee and distribute to the more “normal” side of the knee.
Good shoes: Well made shoes that fit well can help to reduce shock on the knee.
Activity Modification: Also, if you choose walking as your primary exercise, try to walk on surfaces like cinder (found on running tracks), sand, or grass. Cement, asphalt or other hard surfaces may increase the stress on your knees and irritate them. Slow down if increasing your walking speed irritates your knee. Other exercises that are more gentle on the knee include riding a stationary bike, water aerobics, and swimming.
General fitness: The Surgeon General recommends that everyone get 30 minutes of moderate activity a day for up to seven days a week. Moderate activity can include walking, swimming, stationary biking, or low impact aerobics. These activities can help to reduce the risk of heart disease, lower stress levels, help in the management of body weight, and prolong life.
Ultimately, if you are finding that you are avoiding these activities to avoid knee pain as a result of your knee arthritis, it is important that you discuss management options with your doctor so that you can get back to doing these activities.
Surgical Treatment
The most common surgical treatment for knee arthritis is a total knee arthroplasty. There are a couple of other options, however, much fewer individuals typically qualify for these surgeries.
Proximal Tibial Osteotomy or Distal Femoral Osteotomy
Sometimes only one part of the knee joint becomes arthritic. Most commonly this involves the medial (or inner) compartment of the knee. In about 1 of 10 patients, it primarily involves the lateral (or outer) compartment. Typically, when this occurs, the normal weight bearing axis of the knee begins to shift towards the affected compartment, making the problem even worse.
In these situations, it may be possible to re-align the knees to shift more weight away from the affected compartment. This, presumably places the majority of the weight-bearing force into a healthier compartment. The result is to reduce pain and to hopefully delay the progression of joint degeneration.
There are two procedures that can be performed to accomplish this: a proximal tibial osteotomy or distal femoral osteotomy. In these procedures, a wedge is surgically made into either of the two bones (tibia or femur — depending on the deformity). The main advantage to these approaches is that very active people get to keep their own knee joint and once the bones heal there are typically no restrictions to activity level. In the younger, more active patient, this may be a reasonable option to consider if painful arthritis is truly limited to a single compartment of the knee.
Partial Knee Replacement (Unicompartmental Knee Arthroplasty)
Another surgical treatment for arthritis limited to a single compartment is a unicompartmental knee arthroplasty. In this procedure, the arthritic joint surface of the involved compartment is replaced. Compared to a total knee replacement, recovery is typically much faster and requires less rehabilitation. Furthermore, the replacement may feel more like your normal knee because only a small portion of your knee is being replaced.
Total Knee Replacement
The final solution for generalized osteoarthritis of the knee is to completely replace the joint surfaces with an artificial knee joint. The decision to go ahead with a total knee replacement is ultimately your own. When knee replacement surgery is considered the right option for you is typically when all non-surgical treatments have stopped working for you and you decide that the risks of surgery are worth the benefits of a knee replacement surgery. Therefore, it is strictly an elective surgery and there are only uncommon situations where your surgeon may recommend more early knee replacement.
Typically, total knee replacement surgery is reserved for older individuals. The main reason that orthopedic surgeons are reluctant to do a knee replacement in younger people is that the implants themselves have limited life spans. Also, as younger individuals tend to be much more active, they tend to wear through these implants faster. Replacing a failed artificial knee (revision knee arthroplasty) is typically a larger surgery and associated with more risks than a primary total knee replacement surgery.
