Your Baby
Weeks 27 to 31
Your baby’s weight has almost doubled over the past month. She has grown about 3 inches longer, and weighs nearly 3 pounds. The hair on her head is beginning to grow longer. Any nutrients she doesn’t use for energy or growth will be stored as fat under her skin. Her body is becoming plump and round during this process. Her nervous system also now begins to regulate all of the functions of her organs, and control her body temperature.
Over the next few weeks, your immunities will be passed to her via the placenta.
If born at 27 weeks, a baby will need special care from doctors, nurses, and other professionals in a neonatal intensive care unit. These interventions support preterm infants while their brains and organs continue to develop, and their bodies continue to grow and gain weight.
Weight Gain

Pregnancy causes major changes within your body, including effects on your metabolism. Changes in metabolism help you benefit most from the foods you eat to provide your baby with the nutrients, water, and oxygen she needs for healthy growth and normal development.
Gaining enough weight
Gaining enough weight is a sign that the nutritional needs of you and your baby are being met, and helps your baby to also gain weight. Mothers with poor weight gain during pregnancy often have babies who are born too small. In cases of intrauterine growth retardation (IUGR), the baby does not receive enough calories and nutrients to support normal growth. Insufficient maternal weight gain can also result in an infant who is small for gestational age (SGA). These babies are born with a weight that is below the 10th percentile. In both cases, these babies are at risk for physical and developmental problems. Gaining less than the recommended amount of weigh may effect your baby’s chances of being healthy.
Gaining weight at a healthy rate
The rate at which you gain weight is carefully monitored by your doctor. Gaining or losing too much over a short period of time while pregnant can be a sign of a medical problem that can affect the health of the baby. The American College of Obstetricians and Gynecologists recommends the following rates of weight gain for a healthy pregnancy:
Maternal BMI Recommended Weight Gain Per Week
- Less than 18.5 1 lb
- 18.5 to 24.9 1 lb
- 25 to 29.9 0.6 lbs
- over 30 0.5 lbs
These rates are based on the mother’s pre-pregnancy weight and height. For example, if underweight prior to the pregnancy, mothers should gain five pounds during the first trimester, then about one pound per week thereafter. The total weight gain should be 28 to 40 pounds.
Normal weight mothers should gain three to five pounds during the first 13 weeks followed by one pound per week, for a total of 25 to 35 pounds. If overweight, weight gain should be limited to two pounds during the first trimester, and only a half pound per week throughout the remainder of the pregnancy, for a total of 15 to 25 pounds. Women with a BMI over 30 are at risk for having an infant who is either large or small for gestational age. The risk of a premature birth is also higher. For pregnant teen girls, weight recommendations are also based on BMIs due to their increasing rates of obesity. In general, mothers carrying twins should gain 37 to 54 lbs. Underweight women with a twin pregnancy should gain 50 to 60 lbs, and those who are overweight should only gain 31 to 50 lbs.
During the first few weeks of pregnancy, your body begins to store fat from your diet. Most of this of body fat accumulation occurs during weeks 14 through 28. The extra fat is stored on your back, abdomen, and upper thighs; as a result, your pre-pregnancy clothes may not fit even before your pregnancy begins to show. During this increase in maternal body fat, there is very little fetal growth. After 28 weeks, the fat provides a reserve of calories to help your baby grow. It is, therefore, important that your diet keeps up with the nutritional needs of you and your baby.
The weight gain you experience during your pregnancy should be steady. However, if the weight gain is rapid, you should not restrict your calories. Dieting can prevent you from eating enough food to provide your baby with the right nutrients, and result in IUGR or an SGA newborn. It is best to speak to your doctor about what meal plan is ideal for your situation. Instead of dieting, try controlling your weight gain by eliminating sweets and processed foods. If, however, nausea and vomiting from morning sickness cause weight loss or poor weight gain, try to eat more after this phase subsides. In some cases, your doctor may recommend a consultation with a nutritionist. The goal is to gain weight at a healthy rate. An unsteady pattern of weight gain for you means an inconsistent food supply for your baby.
Weigh yourself every day. If you stop gaining or are losing weight, call your doctor. If you gain more than two pounds in one week and develop swelling in your hands, feet, and face, call your doctor immediately.
Monitoring Weight Gain
We have some great tools for monitoring your weight as well as a guide for a healthy diet. These include a daily food guide, pregnancy weight chart, and a 2-day food record.
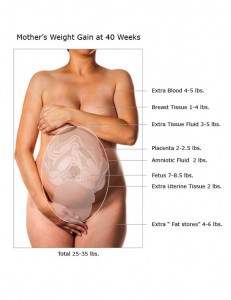
Where the weight goes
Your baby makes up only part of your total pregnancy weight gain. Six to eight pounds become fat stores for energy needed during labor, delivery, and breastfeeding. Additional weight comes from the extra blood, muscle, fluids, and tissue your body makes for you and your baby to use while you are pregnant. On average, most women should gain a total of 25 to 30 pounds. The breakdown of weight gain is as follows:
Baby 7-8 pounds
Placenta 1-2 pounds
Amniotic fluid 2 pounds
Uterus 2 pounds
Increased blood supply 3-5 pounds
Breast Fluid, fat and tissue 10 pounds
Total 25-30 pounds
Fasting
Fasting during the second trimester has been linked to preterm labor. Without enough calories, blood sugar may drop to a very low level, called hypoglycemia. When this occurs, mothers may feel weak or lightheaded. The body responds to hypoglycemia by releasing stress hormones and stored fat into the bloodstream which can stimulate uterine contractions. Fat also breaks down into a chemical called ketones during prolonged fasting. If ketones cross the placenta, they can be harmful to your baby. More research is necessary to determine if intermittent fasting has longterm effects on the baby. To prevent low blood sugar levels, eat several small meals every two to three hours. These should include complex carbohydrates such as whole grain breads, pasta or rice which keep blood sugar steady by taking longer to digest.
The Importance of a Balanced Diet
 A balanced diet is defined as a “proper balance of the quality and quantity” of nutrients and calories we consume. Food quality supplies what our bodies need to make and support all of its components. The quantity of foods we eat affects the energy needs of our body. In order to maintain this balance during pregnancy, you must eat enough of the right foods to meet the needs for you and your baby.
A balanced diet is defined as a “proper balance of the quality and quantity” of nutrients and calories we consume. Food quality supplies what our bodies need to make and support all of its components. The quantity of foods we eat affects the energy needs of our body. In order to maintain this balance during pregnancy, you must eat enough of the right foods to meet the needs for you and your baby.
More caloric energy is necessary for your heart to pump more blood, and for you to carry the extra weight of pregnancy. Your baby needs energy for the heart to beat, nerves in his brain to connect, and the organs and body to grow. As he gets larger, calories are needed for arms and leg movements. Carbohydrates and fats are the main food energy sources. Proteins can also provide energy, but are primarily used for organ, muscle, and tissue building as well as cell repair. Getting enough calories to meet these energy needs is extremely important during pregnancy. Without enough calories, the body will try to obtain nutrients from your muscles or bones to support the growing baby.
Our daily energy and body building needs are best met by eating the six essential food nutrients: proteins, carbohydrates, fats, vitamins, minerals, and water. The FDA recommends a daily intake of vegetables, fruits, whole grains, healthy fats, proteins, and a calcium source. In addition to dietary sources, specific vitamins and minerals are recommended for pregnant women. Except for vitamin D, most are obtained from the foods we eat.
Iron Deficiency Anemia
Iron is important for fetal muscle and brain development, and making hemoglobin. This essential blood protein carries oxygen where it is needed throughout your body, and to your baby via the placenta. Anemia is a common nutritional problem during pregnancy. Its symptoms include constant fatigue, dizziness, rapid heartbeat, and pale skin. Preventing anemia during pregnancy is important because it can cause preterm birth, low birth weight, and problems for the mother during childbirth. Also, feeling tired all the time can affect your mood, making it more difficult to do what is necessary to stay healthy during your pregnancy. It can increase feelings of stress, and decrease your ability to cope.
Anemia can be prevented by eating foods that are rich in iron, and by taking prescribed iron supplements. Iron and other prenatal vitamins should be taken with foods or beverages that are high in vitamin C to increase intestinal absorption. Taking them with meals may also reduce side effects such as nausea or stomach discomfort. Avoid taking iron supplements with milk products as they can reduce the amount of iron that is absorbed.
Excellent Sources of Iron
2 oz. calf or beef liver
1 cup pumpkin or chia seeds
1/4 cup prunes or prune juice
1 cup mustard greens or kale
1/2 cup dried raisins
1 cup spinach
1/2 cup of fortified cereal
2 oz. lean beef
1 cup beans or lentils
2 oz. clams
2 eggs yolks
Folic Acid (Folate)
Folic acid is a B vitamin. Your body uses it to form DNA, for cell division, and to make the extra blood cells needed during pregnancy. It is also important for the formation of the brain and spinal cord of your baby. When the fetus doesn’t get enough folate, the brain or spinal cord may not form properly, resulting in a neural tube defect. Such abnormalities include spina bifida, a leading cause of paralysis in children, and anencephaly, which is fatal. The best sources for folate are dark leafy green vegetables, romaine lettuce, asparagus, broccoli, orange juice, liver, sunflower seeds, cauliflower, wheat germ, and cabbage. Because some food preparations can destroy folate, it is better to eat the fruit and vegetable sources raw, or prepare them with a minimum amount of water (i.e. steaming, stir-frying, microwaving).
Most women are unable to consume enough folate from dietary sources, so doctors prescribe a supplement. It is recommended that women take 400mcg of folate starting one month prior to becoming pregnant, and to continue it throughout the pregnancy. Most prenatal vitamin formulations contain folate.
Calcium, Phosphorus, and Vitamin D
Calcium and phosphorus are necessary for the formation of bones, blood clotting, various cell functions, and muscle contractions. Vitamin D functions like a hormone to promote the absorption of calcium into bones, and support the immune system. It may also prevent high blood pressure and sugar levels during pregnancy. All three of these essential nutrients are important during weeks 27 through 40 when rapid fetal growth occurs, and bones and teeth develop. Food sources of calcium often contain phosphorus and vitamin D as well. Nonfat milk is the best source, but many plant-based milks are fortified with these ingredients. Check food labels to be sure. Eating the recommended servings of milk, yogurt, cheese, eggs, fish, or tofu can supply the extra calcium, phosphorus, and vitamin D needed during pregnancy.
Excellent Food Sources
1/4 cup powdered skim milk, dry
1 cup buttermilk
1/2 cup evaporated whole milk
2 oz. sardines
1 cup yogurt
1/2 cup raw mushrooms
1 cup skim or low fat milk
1 oz. cheddar or swiss cheese
Constipation
Constipation is a common problem during pregnancy, especially when on bed rest, or your activity level has been reduced. It may also be difficult to pass stools due to the pressure of the growing uterus on your rectum. If you are having fewer than three stools per week, it may be time to speak to your doctor.
Tips for preventing constipation:
~ Eat more high fiber foods such as raw fruits, vegetables, and whole grains.
~ Drink six to eight 8-ounce glasses of water every day.
~ Drink hot water mixed with one tsp of lemon juice three times a day.
~ Eat meals at “regular” times.
~ Kiwi fruit, dried or stewed prunes, prune juice, raw carrots, bran or bran cereals, and fresh or dried figs are excellent foods for preventing or relieving constipation.
Unhealthy Habits
Your pregnancy is a perfect opportunity to discontinue an unhealthy habit.
Smoking
Pregnant women who smoke or are exposed to it have an increased risk of an ectopic pregnancy, vaginal bleeding, miscarriage, stillbirth, preterm birth, cesarean birth, or fetal death. This includes the use of tobacco products and e-cigarettes. Nicotine reduces the blood supply to the placenta, so the baby receives fewer nutrients. It also lowers the amount of oxygen in the blood and increases the level of carbon dioxide. These two factors can result in babies who are born too small or prematurely. After birth, these infants have a higher risk of sudden infant death syndrome (SIDS). If you smoke or vape, try to quit or decrease the amount and frequency. Talk with your doctor before trying a nicotine patch.
Drugs and Alcohol
Drinking large amounts of alcohol can cause fetal alcohol syndrome, a constellation of birth defects and abnormal brain development. In the past, there was a belief that “light drinking” may not harm the developing fetus. However, there is no clinical proof of this. The current consensus among health authorities is that no amount of alcohol exposure is safe, and it should be avoided if planning to become pregnant.
Drugs such as marijuana, cocaine, crystal meth, heroin, fentanyl, methadone, and amphetamines have adverse effects on the baby’s brain development and physiology. They may also trigger withdrawal symptoms after birth. Because it causes vasoconstriction, cocaine reduces the mother’s blood supply to her uterus, preventing nutrients and oxygen from getting to the baby. Marijuana use during pregnancy can increase the risk of prematurity, SGA, or fetal death.
All of these substances are passed from your bloodstream to your baby. Unfortunately, a baby’s developing liver and kidneys cannot efficiently eliminate them from the body, causing accumulation and toxic effects. If you have problems with alcohol or drugs, speak with your doctor.
Many over-the-counter medicines should also be avoided during pregnancy, including ibuprofen and some “cold” remedies. Always ask your doctor before taking any new medications, including prenatal vitamins.
Caffeine
Clinical research on the effects of drinking caffeinated beverages while pregnant has produced mixed results. Previous studies stated that moderate consumption of caffeine, as in one or two cups per day, did not pose a significant risk to the unborn baby. However, recent studies indicate otherwise. During pregnancy, a mother’s ability to metabolize caffeine decreases, so it remains in the bloodstream longer. It then easily passes through the placenta to the baby who has no ability to metabolize it. Caffeine is also a stimulant and diuretic which can reduce the flow of blood from mother to baby. As a result, consumption of caffeinated beverages increases your baby’s risk of IUGR, low birth weight, and future developmental delay or obesity. It also increases the risk of a miscarriage. Too much caffeine can also cause your newborn to have withdrawal symptoms. For these reasons, pregnant mothers should avoid caffeine, and even low amounts of consumption are associated with adverse outcomes.
During your pregnancy, avoid coffee, cocoa, colas, teas, and energy drinks. If giving up coffee “cold turkey” gives you a headache, cut back gradually. Decaffeinated coffee and tea is available in most grocery stores, however, water and low fat milk are better beverage choices. In addition, some over-the-counter medicines contain caffeine; these should be avoided as well.
