The growing interest in exercise and sports has made knee injuries increasingly common.
Arthroscopy allows your surgeon to see into the knee joint and to address injuries in a more minimally invasive manner than was traditionally possible. Arthroscopy can be used to treat meniscal and ligament injuries, wear and tear problems, and to remove loose bodies within the joint. Healing time is typically quite short, scarring minimal, and patients usually go home on the same day as their surgery.
Check here if you are looking for information about total knee replacement surgery.
These are some of the problems that can be surgically treated with arthroscopic knee surgery:
• Synovitis—inflammation of the synovial membrane
• chondromalacia
• meniscal tears
• ligamentous injuries or tears
• loose bodies
• knee instability
This article teaches you about knee anatomy, common knee problems and knee arthroscopy. The content and medical illustrations in this article are property of Media Partners, Inc. and have been filed with the U.S. Copyright Office.
Healthy Knee Anatomy
Knowing knee joint anatomy can help you to understand your knee problem better. It can also help you to properly care for your knee after your surgery. Proper care often helps shorten your recovery time and improves your surgical outcome.
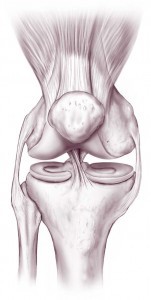
A joint is typically formed where two or more bones meet. The four bones that meet with one another to ultimately form the knee joint are the kneecap (patella), thighbone (femur), fibula, and shinbone (tibia).
The parts of the bones that touch each other are covered with articular (or hyaline) cartilage. This cartilage is a smooth cushion that helps to protect the bones. The cartilage creates an almost frictionless surface that allows for painless and free motion of the bones against one another.
The synovial membrane is a thin layer of tissue that lines the inner aspect of the entire knee joint. It produces a substance called synovial fluid. Synovial fluid is a slippery substance that keeps the joint lubricated and allows for even greater freedom of movement.
The knee joint has two menisci (singular: meniscus) that sit one top of the tibia. Each meniscus is made up of fibrocartilage, a rubber-like tissue. The menisci act as shock absorbers and also help to improve the stability of the knee joint. When significant portions of the menisci are damaged or removed, the articular cartilage usually ends up wearing down more quickly, leading to early arthritis.
Ligaments are rope-like bands of tissue that connect and support the bones of a joint. Several ligaments span the knee and act to keep it stable.
Tendons are elastic tissues that connect muscles to bones and enable a muscle to move bone when it contracts. The muscles of the knee and their associated tendons help to further stabilize the knee.
Knee Problems and Repairs
Knee problems can be caused by disease or by injury. Symptoms can include pain, swelling, instability, clicking, catching, locking, and difficulty walking.
The most common knee problems are:
- Torn ligaments
- Meniscal tears
- Loose bodies
- Arthritis or chondromalacia
- Tendonitis
- Bursitis
Torn Ligament
There are many ligaments around the knee that help to stabilize it. These include the medial collateral ligament (MCL), lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and the posterior cruciate ligament (PCL).
Sudden start-stop movements and quick changes in direction are common movements during which ligamentous injuries can occur. These types of movements are commonly used in basketball, football, soccer, and skiing.
Sudden tearing of a ligament may cause pain, swelling or difficulty in walking. More commonly, ligamentous tears may make the knee feel unstable.
Ligamentous injuries range from sprains (stretching or partial tearing) to complete tears. Ligament sprains or even some tears are often able to be treated without any surgery, taking anywhere from 4 weeks to several months to fully heal. On the other hand, a torn ligament that requires reconstructive surgery can take months to even a year to fully heal.
Some ligamentous injuries (most often tears of the ACL) are associated with meniscal tears.
Ligament Reconstruction
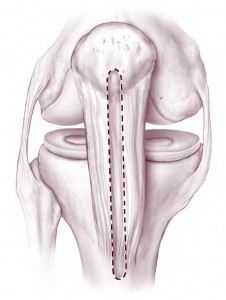
If you tear a ligament and it cannot be treated without surgery, surgical reconstruction of the torn ligament may be the next step. Typically at this stage, imaging studies including a MRI will have been ordered to evaluate your injury and to plan for surgery.
Which reconstructive option will be best for you depends on the type of injury you have sustained. Additionally, there are numerous ways to reconstruct each ligament.
For instance, if you tear your anterior cruciate ligament (ACL), reconstruction (versus repair i.e. tying the two torn ends together) of the ACL is the current standard of care. Your ACL can be reconstructed using donor (cadaver) tendon (allograft) or using your own tissue (autograft). There are various autograft options available that can be used to reconstruct your ACL (hamstrings, patellar tendon, quadriceps tendon), each with its own pros and cons.
Ultimately, the method used to reconstruct your ACL will depend on your age, activity level, and goals of surgery. This is true of any ligamentous repair that you and your surgeon decide to reconstruct (MCL, LCL, PCL).
Finally, ligamentous injuries are often associated with meniscal or cartilage injuries. These are oftentimes concomitantly addressed at the time of surgery if the surgeon thinks that it is necessary.
Its important to remember that ligaments take a long time to heal. You may have to limit the amount of weight you put on your knee or motion around the knee for several weeks after a ligament reconstruction. You’ll likely need crutches to get around initially and your surgeon may ask that you wear a brace to help support your knee while it heals. At some point, strength and range-of-motion exercises will be needed to get your muscles strong enough to support your knee. It can sometimes take up to a year to get back to your normal activities.
Torn Meniscus
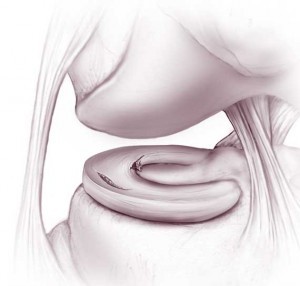
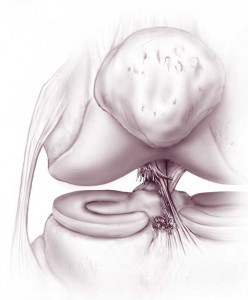
Meniscal injuries can occur after forced twisting of the knee (acute meniscal tears). This can happen during sports or even during normal daily activity. The meniscus also becomes softer with age, making it easier to tear. Meniscal tears can also occur in the setting of arthritis (degenerative meniscal tears).
A torn meniscus can cause catching or locking of the knee, giving way or buckling (instability) of the knee, pain or swelling. The size, location, chronicity of the tear as well the presence of any additional injuries will help to determine both treatment and recovery. If you and your surgeon decide that surgery is the next step, treatment of meniscal tears typically includes either partial removal or repair. Whether the meniscus is repaired or removed will depend on many factors including your age, any additional injuries or associated arthritis within the knee, and the pattern of tear. Ultimately, the final decision to repair or partially remove a meniscus is made by the surgeon at the time of surgery when the injury is directly visualized with the arthroscopic camera. It is only then that the surgeon can truly understand if the tear is repairable.
It is important to remember that not all meniscal tears require surgery i.e. just because somebody says there is a meniscal tear on your MRI, doesn’t mean that you need surgery. Understanding when surgery is needed will depend on your symptoms, your age, any additional injuries, and your ultimate functional goals. Only you and your orthopedic surgeon can make this decision together.
Chondromalacia
Chondromalacia can be caused by overuse or injury to the articular cartilage of the knee joint. This results in softening of the articular cartilage. It most commonly occurs underneath the patella (knee cap) where the patella rubs with the end of the thigh bone (femur). As the cartilage softens, it wears away more easily during joint movements. The cartilage can also just thin with age. Both of these can result in loose pieces of cartilage that cause catching or locking of the knee, giving way or buckling of the knee (instability), pain or swelling. As chondromalacia most often involves the patellofemoral compartment (the underside of the patella), the most common symptom is front of knee pain with walking down hills or stairs or pain after prolonged sitting in chairs.
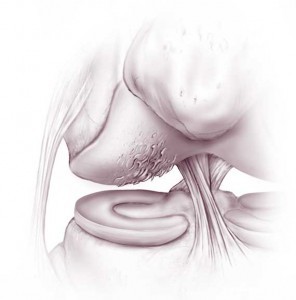
Anti-inflammatory medications (NSAIDs) and physical therapy to stretch and strengthen the hamstrings and quads are the mainstays of treatment for chondromalacia and should almost always be tried before choosing to have surgery. Although uncommon, if medications and physical therapy don’t help, surgery may be warranted.
Surgical treatment will depend on how much cartilage is involved and your symptoms. Treatment may include smoothing or shaving down the loose cartilage (chondroplasty) combined with other techniques such as microfracture, etc. Your surgeon will be discuss with you which type of surgery will be most beneficial for you.
Depending on the type of surgery that is performed, post-surgical recovery can take from weeks to months.
Loose Body (Joint Mouse)
Any free-floating object in the synovial fluid of the knee is known as a loose body or joint mouse. It can be a fragment of bone, cartilage, or meniscus. It can also be a piece of glass, metal or any foreign object. A loose body isn’t usually noticeable until it lodges somewhere in the joint. Your symptoms can change depending upon the exact location of the loose body within your knee. A loose body can cause catching or locking of the knee, giving way or buckling of the knee (instability), pain or swelling.
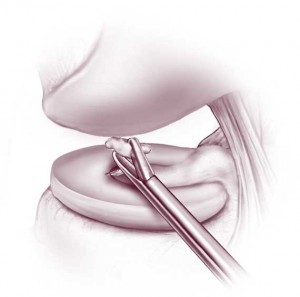
Arthroscopy allows your surgeon to find the loose body in your knee joint and to remove it.
What is Arthroscopy?
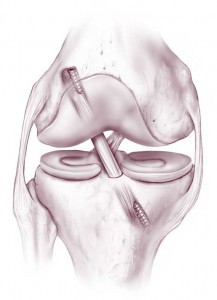
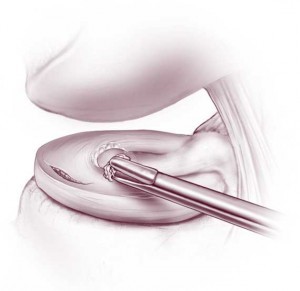
 Now that we’ve talked about some of the more common knee issues that can be addressed with arthroscopy, let’s talk more about what arthroscopy actually is. Arthoscopy allows the surgeon to visualize the inside of the joint and address any issues within it.
Now that we’ve talked about some of the more common knee issues that can be addressed with arthroscopy, let’s talk more about what arthroscopy actually is. Arthoscopy allows the surgeon to visualize the inside of the joint and address any issues within it.
At the start of an arthroscopic surgery, a small incision is made to enter the knee joint. The arthroscope—a tube with a tiny video camera on the end—is then inserted into the knee joint. The arthroscope has fluid in-flow as well as a light on the end of it. The sterile fluid that flows through the arthroscope and is pumped into the knee expands the joint space and allows your surgeon to see your joint more easily. The pressure of this fluid also helps to control bleeding.
The inside of your knee joint is now viewed on a video monitor. Several more small incisions may be made around the knee allowing for the insertion of other instruments. Commonly used instruments are: forceps, scissors, a blunt hook, a shaver and a burr. These instruments are used to grasp, repair or remove bits of tissue or bone.
Depending on what needs to be done, the surgery itself can last between 30 minutes to several hours. At the conclusion of the surgery, the fluid is drained out. As the surgeon finishes, your incisions are closed with sutures or adhesive strips. Then your knee is bandaged with a compression bandage to reduce swelling and bleeding.
Because only small incisions are made, arthroscopic surgery is an outpatient procedure. This means that you can go home the same day that you have your surgery.
Getting Ready for Surgery
Since arthroscopic knee surgery usually is not performed in an emergency setting, you will have plenty of time to prepare. Your surgical team will likely give you instructions on what to do in the 2 weeks before surgery.
In the weeks / days prior to surgery:
• Tell your surgical team about any and all medications you are currently taking — including non-prescription medications, supplements, or herbs
• You will likely need to stop taking any medication that makes it harder for your blood to clot. These include: aspirin, plavix, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), warfarin (Coumadin), xarelto, pradaxa. Rarely, your doctors may ask you to continue taking these medications around the time of surgery. Therefore, it is always best to check with both your surgical team and primary care doctor to see what they recommend.
• Ask your primary care doctor which of your daily medicines you should take on the day of surgery.
• If you smoke, try to quit. Ask your primary care doctor for help quitting—but don’t use a nicotine patch. Smoking (nicotine) can slow down wound and bone healing and can increase your risk of developing a wound infection.
• If you develop an illness or infection prior to surgery, be sure to call and let your surgical team know. If this is the case, sometimes your surgery will have to be postponed until a later date for your safety. It is better to know sooner than later so your surgical team can get you rescheduled.
• Let your surgical team know of any abrasions, cuts, or wounds that you may have sustained around your knee. These can increase the risk of infection after surgery, and as such, surgery may need to be postponed.
• Get your home ready for your return home. Depending on what type of surgery is being performed, it may be best to set up an area within your home where you won’t have to go up and down stairs. Rearrange furniture so you can easily get around with crutches.
• If possible, strengthen your leg muscles with exercises. In fact, depending on what surgery is planned for you, your surgeon may actually require that you do some therapy prior to surgery to improve your range of motion and strengthen your muscles. This will help with your post-operative rehabilitation.
The day before surgery:
• Shower the night before surgery and make sure that your knee is nice and clean.
• Do not drink or eat anything after midnight the night before surgery
On the day of surgery:
• Take any medications that your primary care doctor said were okay to take the day of surgery with small sips of water
• Get to the hospital or surgery center early. You will likely have to show that you have brought someone with you that can drive you home after surgery
• Wear loose fitting clothing that can accommodate a brace or bulky bandage over the knee. Sweat pants or basketball shorts are good choices.
• If you were given crutches, cane or a brace before surgery, bring this with you.
Pre-operative Area
After checking in for surgery, you will go to the pre-operative area. Your blood pressure, heart rate, breathing rate, and temperature are typically closely monitored. You will likely meet your anesthesiologist here. An intravenous line (IV) may be placed into your arm or hand. The IV allows for medications and fluids to be directly administered into your bloodstream before, during, and after surgery.
• Tell your anesthesiologist if you drink more than 1 or 2 drinks of alcohol a day
• Your surgeon will ask you to sign a surgical consent form if you haven’t signed one already. By signing the consent form, you are saying that you understand the risks, benefits and possible alternatives to surgery and that you give your permission to go ahead with surgery
Anesthesia
The three types of anesthesia used for arthroscopy are:
• local anesthesia—numbs your knee area
• regional anesthesia—numbs the leg
• general anesthesia—puts you to sleep
Usually, a combination of regional and general anesthesia are used. Regional anesthesia or a “block” will give you continued pain relief even after you wake up. With general anesthesia, the goal is that you are asleep during the surgery and that you don’t remember the surgery at all.
Recovery Room
At the end of your surgery, you will be taken to the recovery room. You will be in recovery until the effects of anesthesia have worn off (usually a few hours), you’re past the time point where complications are likely to occur, and you’re reasonably free of pain. You can usually have a visitor in the recovery room.
Your blood pressure, heart rate, breathing rate, and temperature are closely monitored. You may be given fluids and medicines to help control pain or nausea associated with general anesthesia. You’ll likely have an ice pack on your knee to help keep down the swelling. Your surgical leg circulation and sensation are checked by the recovery room nurses.
Discharge – Going Home
Your surgical team decides when you’re ready to be discharged. Discharge is based on your recovery from anesthesia and whether your pain is adequately controlled. If any problems arise in the recovery room or you need to be watched longer, you may be admitted to the hospital. When you’re discharged, someone will have to drive you home.
You may have a big bandage, brace, or ice pack on your knee that goes home with you. A nurse usually reviews post-operative instructions with you, gets your prescriptions, tells you when to make a follow-up appointment with your surgeon, and what to do if you have any problems when you get home. If you had a nerve block, it may take several hours to regain feeling in the affected leg.
Recovery At Home
Knowing how to care for your knee once you get home will make a big difference in your recovery and results. How fast your knee heals depends highly on the surgery performed, your age, your health, your fitness level before surgery, how active you are or want to be, and how much time you’re willing to spend on getting your knee back to normal.
Before going home, your surgeon may give you a set of instructions similar to these:
• Help at home: For the first 24 hours after surgery you should not be left alone. This is if you need help or if any unforeseen problems arise. Remember, you cannot drive immediately after surgery.
• Rest and walking: You may feel groggy for the first 24-48 hours following surgery. Rest and give your body time to recover from surgery and anesthesia. Be sure to wear your brace if your surgeon instructed you to wear one. Use your crutches or other assistive devices, as directed. Be careful not to trip and fall. Keep your hands free to help you balance.
• Weight bearing: Your surgical team will have explained to you if you can or cannot put weight on your surgical leg.
• Medicine: Take all medications as prescribed by your surgeon. You may typically resume any of your normal home medications unless otherwise directed by your surgical team
• For pain and swelling: Your knee is likely to feel sore and be swollen for at least a week. Ice your knee as directed. While lying down, elevate your knee so that it rests above the level of your heart as much as possible. Take pain medicine as prescribed. (See R.I.C.E. Therapy)
• Crutches: Use assistive devices as directed by your surgeon.
• Wound care: Keep your wound and bandage dry and clean. With your surgeon’s permission, you may remove your bandage a few days after the surgery. At this time, you may typically shower as usual—use a nonslip mat and hand rails when possible until your knee is strong and stable. Do not soak your incisions in a bathtub. Check your incision every day for redness, tenderness, or drainage. It is normal to see some bruising of the wound with some associated swelling of the leg.
• Exercise: Begin a strengthening and range of motion exercise program as instructed by your surgeon or physical therapist. Don’t forget to ice your knee after therapy.
• Return to routine: Return to daily activities and work as directed by your surgical team. Return to more vigorous activities once cleared by your surgeon.
When to call your Surgeon:
Call your surgeon to make or confirm a follow-up appointment.
Call your surgical team with any questions you have about your healing process or if you notice any of the following:
• continued bleeding through the bandage
• A fever over 101.5ºF or if you have shaking chills
• Continued bleeding through the bandage
• Persistent swelling, warmth or redness around your knee
• Tingling in your toes that does not improve, or if they become cold, discolored or numb
• Persistent or increasing pain, not relieved by your pain medication or with rest
• Pain, swelling or tenderness in your calf
• Headache, muscle aches or dizziness
• Trouble breathing or chest pain
Call 911 if you have chest pain, shortness of breath, or severe nausea after surgery
Expectations After Arthroscopy
Recovery Time
The amount of time it takes to fully recover after surgery depends on what was done during your surgery. If a “smaller” surgery such as a simple loose body removal was performed, recovery can be as short as a matter of weeks. If a large reconstructive surgery was performed, it may take up to a year for your knee to make a full recovery. The time needed for recovery also depends upon your age, your fitness level, and any other medical issues that you might have. After knee arthroscopy, you will have small scars on your knee from the incisions used to perform the surgery.
Frequently Asked Questions After Arthroscopy
- There is blood and drainage from the incisions. Is that OK? A little drainage that is watery and clear or reddish in color is common for the first few days following surgery. If the drainage is bright red or looks like pus and is associated with a fever and/or pain, call your surgeon right away.
- What if I have a slight fever? It’s normal to have a slight fever immediately after surgery. Take some Tylenol, aspirin, or ibuprofen as directed for the fever. If the fever is above 101.5F, or persists for more than a day after surgery, call your surgical team.
- When can I take a shower or bath? Keep your surgical wounds dry for a few days. Typically, you may shower after that and let water run over your wounds. Typically, no scrubbing or soaking of the wounds is allowed for several weeks. Ultimately, confirm these facts with your surgical team before and after surgery.
- When can I move around? You should be up and moving around as soon as you can after you recover from anesthesia. To prevent falls, you should not try to walk around unassisted while on narcotic pain medicine. Use assistive devices while on narcotic medications. Ultimately, good mobility after surgery will help to prevent blood clots and keep your lungs healthy.
- Why is my skin itching? Likely this is a side effect of the narcotic pain medication. Narcotic pain medications can make you feel itchy. Unless you develop a rash, hives, or shortness of breath, you probably are not having an allergic reaction. You can take an over-the-counter anti-histamine like Claritin or Benadryl to stop the itching. If you are having trouble breathing, call 911.
- Why am I constipated? A side effect of narcotic pain medicines is constipation. This is usually temporary. Also, your lack of activity can add to the problem. You can increase the amount of water, fruit, and fiber you eat. If you need it, take a stool softener. Drink plenty of water. Try to get up and move around as much as you can.
- When can I drive? This really depends on the type of surgery that was performed. Ask your surgical team when you are able to go back to driving.
- When can I go back to work? This also really depends on the type of surgery that was performed. Ask your surgical team when you are able to go back to work.
Questions to Ask Your Surgeon About Arthroscopy
• Should I take my daily medicines before surgery?
• How much pain can I expect after surgery and how will the pain be controlled?
• Will I need crutches or a walker following surgery? For how long? Where can I get these? Should I get them before surgery? Should I bring them to the hospital with me?
• Will I need a brace? For how long? Where do I get one? Should I get it before surgery? Should I bring it to the hospital with me?
• How soon will I be able to drive?
• How soon until I can get back to my normal activities?
• How soon can I go back to work?
• How soon until I can get back to more strenuous activities like sports or exercise?
Write down your questions and the answers to these question so you don’t forget.
Risks of Having Surgery
Knee arthroscopy is generally very safe. However, surgery always has risks. The risks associated with knee arthroscopy include:
• Infection of the surgical wounds
• Blood clots in your legs
• Knee stiffness
• Failure of repair
Some of the risks associated with surgery are specific to your knee problem and your surgery. Be sure to ask your surgeon which risks are relevant for you.
Note that the information in this article is purely informative and should never be used in place of the advice of your treating physicians.
