If you are considering breast reduction surgery, called reduction mammaplasty, you have probably suffered for years from one or more of the medical or other physical problems that many women have who have large breasts. Most women complain of back and neck pain, poor posture, skin irritation and infections, shortness of breath, shoulder strain, indentations from bra straps, inability to play sports or take part in recreational activities, and inability to find clothing that fits causing them to feel self-consciousness and embarrassed about their appearance. Breast reduction is a commonly performed reconstructive surgery removing excess fat, tissue, and skin of large breast and includes reconstruction of the shape of the breast. It may also include reducing the size of the areola, the darker skin surrounding the nipple. The result is smaller, lighter, firmer breasts that are more in proportion with the rest of your body.
This article answers many general questions about breast reduction surgery. Share this booklet with your partner. It explains what to expect before, during and after breast reduction surgery. But, it cannot answer all the questions you might have about your surgery. However, your surgeon can answer any questions you and your partner still have after reading this booklet. This booklet is not meant to replace the advice of your doctor, surgeon or nurse.
The Best Candidates For Breast Reduction
A breast reduction is usually performed to relieve physical and emotional discomfort, not simply for cosmetic improvement. If you have very large, sagging breasts that cause you physical discomfort or pain and that have restricted your activities, you’re probably a good candidate for this surgery. Breast reductions are usually performed on women whose breasts are fully developed. Only in cases of severe physical discomfort would breast reduction be performed on very young women whose breasts are still developing. The best candidates are women mature enough to understand the entire surgical procedure and who have realistic expectations of the results. It is not recommended for women who intend to breast-feed.
Talk With Your Partner
The decision to have breast reduction surgery is a very personal one. However, don’t forget to include your partner in your decision-making process. If you haven’t done so already, talk with your partner about the reasons why you are considering surgery and what your expectations are. Ask for your partner’s opinion about the change in your breast size and shape. Ask your partner to go with you to see the surgeon so you can both have the same understanding of the benefits and risks of surgery.
Talk With Your Benefits Manager or Insurance Provider
Before surgery, find out if breast reduction surgery is covered under your health care plan, and what documentation must be provided to make a determination about coverage. If coverage is provided for certain circumstances, your surgeon’s office will be able to supply the necessary documentation.
Your Visit With The Plastic Surgeon
During your consultation with the surgeon, you should discuss openly and frankly about your reasons for wanting this surgery as well as your expectations. Carefully consider your surgeon’s opinion and recommendations. If surgery is recommended, make sure you are in agreement about the desirable size and shape of your new breasts. Don’t be embarrassed to take magazine pictures with you. Your surgeon will look at and measure your breasts. A photograph will probably be needed for insurance purposes. Your surgeon will talk with you about the surgical procedure, explain the risks of having the surgery, along with any variables that may have an effect on your surgery such as your age, the size and shape of your breasts, and the condition of your skin.
Questions To Ask
Don’t be afraid to ask questions about anything you don’t understand.You probably want to learn as much as you can about your surgery and recovery. The more you know; the more confident you will be about your decision to have surgery and doing your part in speeding your recovery. Try to get your questions answered during your office visit so you know what to expect before surgery.
The following are questions you can ask your surgeon.
• What cup size will my new breasts be?
• How much pain should I expect right after surgery and how will it be controlled?
• How long will I be in the hospital?
• How likely am I to have complications from surgery?
• What can I do before surgery to have the best outcome?
• Should I have a mammogram before or after surgery?
If you think of other questions later, write them down and call your surgeon’s office.
Risks of Breast Reduction Surgery
Breast reduction surgery is not a simple operation, but it is normally safe when performed by a qualified plastic or reconstructive surgeon. As with any surgery, there is a possibility of complications, such as bleeding, infection, or reaction to the anesthesia. With breast reduction surgery, you may develop small sores around your nipples after surgery, which can be treated with antibiotic creams. Breast reduction surgery can also leave you with slightly mismatched breasts, unevenly positioned nipples, permanent loss of feeling in the nipples or breasts and, very rarely, the nipple and areola may lose their blood supply and the tissue will die. The nipple and areola can usually be rebuilt by using skin grafts from other parts of the body. You will have noticeable, permanent scars that can be covered by your bra or bathing suit. Poor healing and wider scars are more common in smokers. Breastfeeding may be a problem later, since many milk ducts leading to the nipples are removed during this surgery.
Possible complications include:
• Abnormal scarring, called keloids. You may need a second surgery for scar revision.
• Small cysts of blood or serum
• Excessive bleeding or blood clots
• Infection of the surgical incision
• Discoloration of healing skin edges
You should talk candidly with your surgeon about the possible risks involved and how you can reduce your risks. Your risks increase with:
• Obesity
• Smoking
• Excess alcohol consumption
• Diabetes
• Poor nutrition
• Some medicines. Be sure to tell your surgeon about any prescription or over-the-counter medicines or supplements that you take. You may need to stop them for a while.
Surgical Consent Form
Your surgeon will ask you to sign a surgical consent form. By signing this form, you are saying that you understand the risks you will be taking (see below for more information) and agree to have the surgery. Ask your surgeon about any concerns you have before you sign this form.
Getting Ready For Surgery
Breast reduction surgery is usually scheduled weeks in advance. Use this time wisely. There is a lot you can do before surgery to make your recovery at home go smoothly. While you are getting ready, carefully follow your health care team’s advice about:
• Whether you should have a mammogram (breast x-ray) before surgery
• Changes you should make in your diet
• Your vitamins and medicines. There may be medicines which you should start, stop, or keep taking. Tell your surgeon about all medicines that you take regularly or occasionally, including prescription medicines, over-the-counter medicines, natural remedies and dietary supplements.
During this time, you should
• Arrange for someone to drive you home following surgery and to help you out for part of the day for the first few days
• Prepare easy-serve meals and freeze them. Stock up on fruit, heat-and-serve soups, and bottled water.
• Buy some supportive bras (but not underwire) or tube tops. You may have to wear a tight bra or tube top 24 hours a day for several weeks after surgery so that your breasts will have good support. Since there may be some drainage from your incisions during the first few days, so buy two or more bras or tube tops so you can change them as often as you need to. Check with your surgeon about estimating cup size for this purpose.
• Make sure you have several button-down-the-front blouses or shirts to wear following surgery and some big, firm pillows
• Also, make sure you have a thermometer, 4’x 4’ sterile gauze pads and Tylenol
• Rest and relax. Take good care of your physical and mental health.
• Report health changes to your surgeon. Tell your surgeon if you have any signs of an infection, such as chills, fever, coughing, or runny nose within a week of your scheduled surgery. If an infection does not go away, your surgery may have to be rescheduled. Also, your surgeon may want your regular doctor to give you a checkup before surgery.
Making Arrangements For Surgery
Plan for a family member or friend to go with you to the hospital for surgery. Even when you are going for pre-admission, it’s a good idea to have someone with you. They can listen and take notes for you—or do some of the walking if that’s what you need! Be sure to give your family member or friend plenty of notice about your upcoming tests and surgery so they can make plans.
List all medicines you are taking and any allergies to medicine or food that you have. Take this list with you when you go to the hospital (for pre-admission and surgery) so you won’t forget anything when asked.
Breast reduction surgery is generally done in a hospital, as an in-patient procedure. The surgery itself usually takes two to four hours, but may take longer in some cases. You can expect to stay in the hospital twenty-four to forty-eight hours.
Pre -Admission Procedures
Generally, a few days before surgery you will need to have certain tests and be ‘pre-admitted’ to the hospital. This pre-admission visit can take several hours. Your surgeon’s office staff will tell you where to go and which tests you will need. You may need:
• A chest x-ray to see how well your lungs are working
• An electrocardiogram (EKG) that shows how your heart is working
• Blood tests that show chemistry and blood counts
• A urine analysis to show how your kidneys are working
During pre-admission you may be asked
• To fill out insurance forms, or give authorization forms from your insurance company; be sure to bring your insurance card if appropriate
• If you brought written orders from your surgeon, lab test results, or paperwork from the blood bank
• The name, address, and telephone number of someone to contact in case of emergency
• To list all medicines you take, including over-the-counter medicine, natural remedies, and dietary supplements
• To list your food and medicine allergies, and how you react to each
You will be told about your rights for advanced directives which are your written directions for your care should you become unable to make decisions. If you have a living will and health care power-of-attorney, bring a copy of these with you.
Anesthesia
An anesthesiologist may talk with you during your pre-admission visit. She will ask about your history with anesthesia and if you are allergic to any medicines.
Breast reduction surgery is nearly always performed under general anesthesia, which means you will be completely asleep during surgery.
If you take daily insulin, heart, or blood pressure medicine, ask the anesthesiologist at what time you should take your medicine the day before and morning of surgery. The anesthesiologist may give you medicine to take before surgery.
Blood Transfusion
Breast reduction surgeries doesn’t usually need a blood transfusion. However, if a large amount of breast tissue will be removed, you may need a unit of blood. If so, the blood you receive is matched with your blood which has been carefully tested. The blood can come from you, a designated donor, or a blood bank. Ask your surgeon which would be best for you.
The Night Before Surgery
Eat a light supper the night before surgery and avoid alcohol. Do not eat or drink anything, except a small amount of water after midnight. This keeps the stomach empty which will reduce nausea and vomiting.
Your Hospital Visit
In the morning before surgery, you can shower or bathe and brush your teeth. Do not eat or drink anything. However, follow your instructions about taking your daily medicine or pre-surgery medicine from the anesthesiologist. When you dress, do not wear makeup, jewelry, dentures, hair pins, contact lenses, or artificial limbs.
Most people are admitted to the hospital the morning of surgery. Follow the instructions given to you during your pre-admission visit about when to arrive at the hospital.
What to Bring to the Hospital
• Your glasses, dentures, or hearing aid, if you use them
• A blouse that buttons down the front or a dress that that you can step into and pull up for when you are discharged
• Any items you were asked to bring during your pre-admission visit
At the hospital, someone will take you to a room or the surgical suite. A nurse will help you get ready for surgery and answer last minute questions. You may be given medicine to make you a little drowsy and relaxed just before you go to the operating room. When you go to surgery, your family will be shown to a waiting area.
Your Surgery
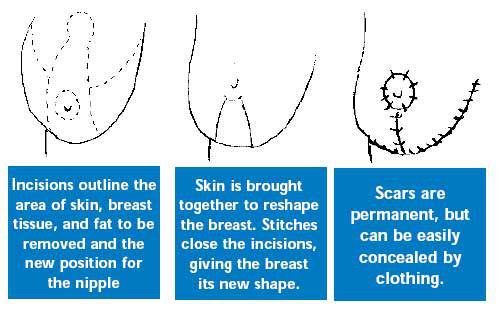
Scars around the areola, below it, and in the crease under the breast are permanent, but can be easily concealed by clothing.Before surgery, an intravenous tube (IV) is placed in your arm or the back of your hand. This tube supplies your body with needed medicines and fluids. Also, you may begin receiving anesthesia through this tube. There are other wires, and tubes attached to or placed in your body. These help monitor your body’s functions, remove excess fluid, and help you breathe during surgery.
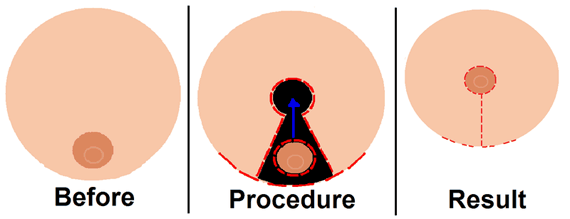
The most common surgical procedure for breast reduction has a keyhole shaped incision that circles the areola, extends downward, and follows the natural curve of the crease beneath the breast. The surgeon removes excess glandular tissue, fat, and skin below where the nipple will be moved to and where the old nipple was. The nipple stays attached to the underlying skin. The surgeon then moves the nipple and areola into their new position. He then brings the skin from both sides of the breast down and around the areola, shaping the new breast. Liposuction may be used to remove excess fat from the armpit area. Drains are left in place to prevent the collection of fluid.
Usually, the nipples remain attached to their blood vessels and nerves. However, if the breasts are very large or pendulous, the nipples and areolas may have to be removed and grafted into a higher position. This will result in a loss of sensation in the nipple and areolar tissue.
Stitches are usually found around the areola, in a vertical line extending downward, and along the lower crease of the breast. Sometimes, techniques can be used that eliminate the vertical part of the scar. And occasionally, when only fat needs to be removed, liposuction alone can be used to reduce breast size, leaving minimal scars. Stitches on the skin are usually removed about 10-14 days after surgery. It can take up to 3 months for your breast to assume their final shape.
After surgery, you’ll be wrapped in an elastic bandage or a surgical bra over gauze dressings. A small tube may be placed in each breast to drain off blood and fluids for the first day or two.
In The Recovery Room
While in the recovery room, you will gradually wake up. You may feel groggy from the anesthesia. You may hear sounds from the equipment around you and your nurse telling you surgery is over. You will still have tubes, and monitors attached. The monitors provide the recovery room nurses with data on how your body is recovering.
The Road To Recovery
Everyone’s recovery rate is different. How quickly you recover depends, partly, on your physical health before surgery and how complex your surgery was. Your greatest discomfort will happen with 24-48 hours after surgery. If you need pain medicine, don’t wait too long to ask for it. It is easier to prevent pain than to stop pain.
The hospital staff will continue your care by checking the fluid coming from your drains, if you have them.
Your part of recovery in the hospital is very simple:
• Make sure your stomach can tolerate fluid before eating solid (bland) foods
• Keep your lungs free of fluid by doing deep breathing and coughing exercises
Prior to being discharged, someone from your health care team will give you discharge instructions, including how to care for your incisions and drains (if you have them), give you a prescription for pain medicine and tell you when to schedule your first follow-up visit with the surgeon. You should take a dose of pain medication about 30 minutes before you leave the hospital and remind a family member to bring a big, firm pillow for you to hold against your chest during the ride home.
When You Get Home
Once you’re home, you may feel some pain for the first couple of days—especially when you move around or cough—and some discomfort for a week or more. Some fluid draining from your surgical wound, or some crusting, is normal. You may have to wear a special “binding” bra for several days to help prevent swelling of your breast. Make sure you change dressing and wear the binding bra it as prescribed by your surgeon. Expect some bleeding or drainage for the first 24 hours. Take all medicines as prescribed—be sure to take antibiotics until you finish the prescription. Take pain medicine as you needed it.
If you have unusual symptoms, such as bleeding or severe pain, don’t hesitate to call your surgeon.
Simple Things To Avoid
Until your doctor says it’s OK, below is a list of activities or other things to avoid while you are recovering:
• You can shower, but don’t soak in a tub where your incisions are underwater. Use mild, unscented soap like Dove.
• Don’t smoke. Smoking drastically retards the healing process and can cause serious complications.
• Limit your arm use to daily activities, such as brushing your teeth, eating, and combing your hair; do not stretch or reach arm above head level.
• Move around and elevate your legs often while resting to reduce the risks of blood clots in your legs.
• Don’t lift anything over 10 pounds; don’t do strenuous household chores or yard work or anything that applies pressure to or pulls on your stitches.
• Don’t sleep on your stomach until soreness has gone away
• Don’t remove the surgical tape, let it wear off. If you have a drain, do not shower until the drain has been removed.
• Use ice packs for the first 24 hours to reduce swelling. Avoid any type of heat to the breast, such as a heating pad, hot compresses for the first 24-48 hours.
• Don’t sun bathe for at least 2 months
• Don’t resume jogging, aerobics or any vigorous exercise for 6 weeks
* Don’t drive for a month
When To Call Your Surgeon
Keep 24-hour phone numbers handy. Call your surgeon’s office if you feel you are not healing as you should—such as the skin edges of the incision separating. Check your incisions every day for signs of infection. If you think you have a fever, take your temperature. If you have signs of infection or other complications, call your surgeon right away.
These are warning signs of infection and other complications
• smelly discharge coming from your incision(s)
• red, hot, and swollen breast(s) or incision(s)
• chills or a fever over 100.4 F
• severe pain in your breast(s) not relieved by pain medicine
• your nipple(s) become markedly discolored
If the signs tell you it’s an emergency and you cannot reach your surgeon, call 911.
Getting Back To Normal
Your first menstruation following surgery may cause your breasts to swell and hurt. You may also experience random, shooting pains for a few months. You can expect some loss of feeling in your nipples and breast skin, caused by the swelling after surgery. This usually fades over the next six weeks or so. In some patients, however, it may last a year or more, and occasionally it may be permanent. Although much of the swelling and bruising will disappear in a few weeks, it may be six months to a year before your breasts settle into their new shape. Even then, their shape may fluctuate in response to your hormonal shifts, weight changes, and pregnancy. Your surgeon will make every effort to make your scars as inconspicuous as possible. Still, it’s important to remember that breast reduction scars are extensive and permanent. They often are lumpy and red for months. Gradually, they fade; eventually, to thin white lines.
Your New Look
Of all plastic surgery procedures, breast reduction results in the quickest body-image changes. You’ll be rid of the physical discomfort of large breasts, your body will look better proportioned, and clothes will fit you better. Don’t worry if it takes you and your family a little time to adjust to your new look. Keep in mind why you had breast reduction surgery. Chances are you’ll be very pleased with the results.