Unfortunately, shoulder injuries are common. A relatively simple and safe procedure, called shoulder arthroscopy, can be performed to diagnose and treat many shoulder injuries and diseases. These surgeries are performed by orthopedic surgeons.
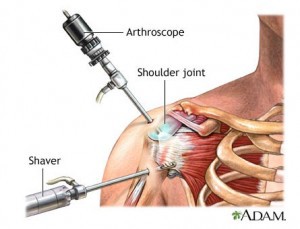
Shoulder arthroscopy is done using a small camera called an arthroscope. The surgeon enters the shoulder with the arthroscope via a small incision. Various surgical tools are used through additional small incisions (called portals) depending on what the surgeon decides needs to be done.
Nowadays, many shoulder surgeries are performed arthroscopically instead of open (bigger incision, no scope) because there is a smaller chance of infection and the shoulder tends to heal more quickly.
Anatomy of the Shoulder
The shoulder is a ball-and-socket type joint where the arm joins the upper thorax. The head (ball) of the humerus (upper arm bone) and the glenoid (socket) of the scapula (shoulder blade) are both covered by smooth hyaline (or articular) cartilage. Within the joint, articular cartilage is made even more slick by joint lubricant called synovial fluid. Ultimately, when the joint is healthy, motion of shoulder is fluid and pain-free.
There are many muscles and ligaments that help to stabilize and move the shoulder. Unfortunately, many of these structures can become injured and become a cause of shoulder pain or instability.
The rotator cuff is an important group of muscles that help to keep the head of the humerus (ball) in the glenoid of the scapula (socket) and stabilize the shoulder. It also aids in the movement of the shoulder in many directions. Injury or disease of the rotator cuff is common secondary to overuse, injury, or trauma and can cause pain and the shoulder to function poorly.
See Anatomy of the Shoulder for more details.
Fortunately, many shoulder issues can be treated successfully with shoulder arthroscopy.
Shoulder Problems Diagnosed or Treated With Arthroscopy
Shoulder arthroscopy may be done to diagnose or treat various shoulder problems (some are listed below). Firstly, however, your doctor will ask you questions and perform a physical examination on you that will help he or she decide what the next best step is in your care. Oftentimes, imaging studies are ordered: X-rays, magnetic resonance imaging (MRI scan), or computed tomographic (CT) imaging to help figure out what is going on.
It is important to remember that not all shoulder problems require surgical intervention. Many shoulder conditions can be successfully treated with non-surgical therapies like rest, ice, anti-inflammatory medications (for example, tylenol or ibuprofen) or physical therapy.
While there are exceptions to the rule, surgery is usually the answer only if non-surgical treatments don’t work first.
Rotator Cuff Tear or Injury
If surgery is required and depending on how badly your rotator cuff is injured, arthroscopic treatment may consist of a simple cleaning up of the tear (known as a debridement) or a repair. During a rotator cuff repair, the edges of the torn tendons are brought together (if necessary) and small rivets (called suture anchors) are often used to help attach the tendon to the bone. The anchors are usually made of plastic and do not need to be removed after surgery. Typically, if a repair is performed, you will be in a sling and be unable to use your shoulder for a little while. Physical therapy will also be required for recovery.
Again, not all rotator cuff tears or injuries require surgery.
The Glenoid Labrum
Oftentimes, after a shoulder dislocation, the glenoid labrum is torn. A shoulder dislocation occurs when the head of the humerus is forced out of the glenoid. This usually occurs after a fall or other traumatic event. This may result in shoulder instability and your shoulder may become painful and feel unstable with specific movements.
Overuse injuries of the labrum can also occur with repetitive overhead motions as well.
Doctors may use words like “Bankart lesion” or “SLAP tear” to describe the above injuries.
Anatomy
The glenoid labrum is a ring shaped structure that is attached to and wraps around the outer glenoid. It increases the depth of the glenoid “socket” by 50% and acts like a bumper to stabilize the joint and prevent the ball-shaped humeral head from coming out of the socket. Importantly, the shoulder capsule, glenohumeral ligaments, and one of the biceps tendon also attach to it.
Tearing of the labrum, that may occur with shoulder trauma or overuse injuries, can lead to pain and other symptoms described below.
Symptoms
Labral tears may be characterized by is a sharp catching type sensation in the shoulder. This may be followed by a vague aching for several hours. This “catching feeling” may occur only with certain movements of the shoulder. Additionally, as the labrum again helps to stabilize the shoulder, a labral tear may make your shoulder feel weak or unstable.
 Diagnosis
Diagnosis
The diagnosis of a labral tear may be suggested by the details of your injury and symptoms (i.e. your history) and the doctor’s physical examination. X-rays maybe often be normal. Magnetic Resonance Imaging (MRI) scan or a Computed Tomographic (CT) Scan with special dye in the shoulder may be used to make the diagnosis. Sometimes, using arthroscopy to look into the shoulder directly is the only way to make confirm the diagnosis.
Treatment
Again, like most other injuries of the shoulder, labral tears may be successfully treated with non-surgical therapies like rest, ice, anti-inflammatory medications (for example, tylenol or ibuprofen) or physical therapy.
In the right situation, or with continued symptoms despite non-surgical therapies, shoulder arthroscopy may be performed to remove or repair the tear.
Shoulder Impingement Syndrome
Impingement syndrome is a condition where structures within the subacromial space become inflamed (including the bursa, rotator cuff) causing pain. Weakness and loss of movement of the shoulder may also be seen. the rotator
If non-surgical treatment is not working, arthroscopic “subacromial decompression” (cleaning out the space between the acromion and rotator cuff) may be performed. During this procedure the irritated bursa and painful bony projections (bone spurs) are removed. This helps to reduce inflammation and pain.
Frozen Shoulder
A frozen shoulder, called adhesive capsulitis, is a condition where the connective tissues surrounding the shoulder joint become inflamed. Is more common in middle-aged females and is often seen in individuals with various hormone issues such as hypothyroidism. It is also more common in diabetics. It may or may not follow shoulder injury.
Frozen shoulder is characterized by pain, then slowly worsening movement restriction (i.e. “frozen”). By far, the most important treatments for frozen shoulder are time and physical therapy. Oftentimes, this condition can take up to 1 to 2 years to fully resolve.
Arthroscopy for frozen shoulder is reserved for select cases and is usually not required. However, in certain situations, it may be beneficial.
Arthritis
Arthritis is a condition in which the cartilage of a joint (articular cartilage) wears down leaving the underlying bone exposed. There are different types of arthritis. The most common type is osteoarthritis. To keep things simple, this type of arthritis can be thought of as your “wear and tear” arthritis i.e. the longer one lives and uses their joints, the more likely the cartilage in the joints will wear down.
Arthritis can lead to painful movement. Typically, the treatment for arthritis is non-surgical. Shoulder arthroscopy is usually not a great surgery for pain secondary to arthritis. However, there are certain select situations where it may potentially be useful.
Torn or Damaged Biceps Tendon
The biceps tendon can oftentimes become inflamed. This is often associated with impingement syndrome or rotator cuff tears. It can also become inflamed on its own. In order to relieve the symptoms of biceps tendonitis, an arthroscopic procedure called the biceps tenodesis or tenotomy may be performed to anchor the tendon (tenodesis) or release the tendon (tenotomy) to treat pain.
Preparing for Shoulder Arthroscopy
Be sure to tell your surgeon about all prescription and non-prescription medicines you are taking, including alcohol, supplements, cigarettes, or herbs. Include the name, the amount and how often you take them. Ask your surgeon which medications to avoid prior to surgery and which you should take on the day of your surgery.
Two Weeks Before Surgery
In preparation for shoulder arthroscopy you may need additional work-up to make sure you are safe for surgery. Typically, your surgeon will have you follow-up with your primary care provider to obtain “pre-operative medical clearance”. Depending on your age and your health, this may consistent of a urine test, various blood tests, an EKG (to check your heart), and chest x-rays to make sure you’re safe for anesthesia.
If you take medications that cause thinning of the blood—like ibuprofen, aspirin, naproxen—you should stop taking these medicines about two weeks before your surgery.
If you are suffering from an illness like a cold, flu, fever, herpes or infection within a week of your surgery, tell your surgeon—your surgery many need to be postponed to prevent complications.
If you smoke or use tobacco products, stop them before surgery. Nicotine slows down the healing process for tissues and bone (i.e. even nicotine patches are not good for healing). Ask your doctor for other ways to help you stop.
If you drink more than one or 2 alcoholic drinks a day, be sure to tell your surgeon.
The Day of Surgery
Don’t eat or drink anything after midnight the day before surgery. Take any medications approved by your primary care doctor the morning of surgery with just a sip of water. Arrive at the hospital or surgical center on time. Usually, it is best to arrive 2-3 hours before your surgery time to prevent any delays.
You will probably go home the day of surgery, so wear clothes that are easy to get on and off. OR bring a family member or friend who can help you. Your shoulder will likely be in a sling so zippers and ties will be all but impossible with one hand. Buttons are OK, snaps are better. Remember that you may not be allowed to raise your arm above your head to put on a sweatshirt or T-shirt. A big shirt or jacket that buttons or snaps up the front will work well. Wear pants that you can slip on and have an elastic waistband, like sweat pants or exercise shorts. Wear shoes, without stockings or socks, that slip on like flip flops, clogs, loafers, or sandals.
Anesthesia for Shoulder Arthroscopy
Usually a combination of both regional anesthesia and general anesthesia is used. The regional anesthesia makes the arm and shoulder numb so you don’t feel any pain during surgery. General anesthesia puts you to sleep and is used to make you comfortable during surgery.
Shoulder Arthroscopy
Shoulder arthroscopy begins with a few small incisions made around the shoulder area. The arthroscope, which is connected to a video monitor, is inserted through one of these incisions. The arthroscope helps the surgeon to get a clear view of the shoulder joint and adjoining cartilage, ligaments and tendons. The other incisions are used for inserting equipment into the shoulder joint which are needed for the repair, reconstruction, etc.
At the end of the procedure, all the incisions are closed with suture, the area is bandaged, and you are taken to the recovery room.
Risks and Complications of Shoulder Arthroscopy
Shoulder arthroscopy is a safe procedure and the chances of complications are low. However, it’s important to know the risks and complications associated with it.
Risks include:
• Bleeding, infection, or blood clots.
• Infection, vomiting, nausea, urinary retention, sore throat, headache from the anesthesia. Some serious effects of anesthesia include strokes, heart attacks and pneumonia.
• Shoulder stiffness or weakness and/or loss of some or all sensation.
• The repair doesn’t heal
• The repair does not relieve symptoms
• Blood vessel or nerve damage in or near the shoulder
Care Following Shoulder Arthroscopy
Care following shoulder arthroscopy depends on the type of surgery that was performed. Make sure you ask lots of questions and get written post-operative instructions before going home. Medications are given to control the post procedure pain.
• Oftentimes following surgery you will have to wear a sling. If and how long you have to wear a sling will depend on the type of shoulder surgery you had. Also, if a repair was performed, usually you will not be able to move the shoulder for a while. Ask your surgical team if and when you can remove your sling (for example, physical therapy or grooming) and what your restrictions are on motion and lifting.
• Apply ice to the area as per surgeon’s instructions either by using an ice machine or putting ice over the bandaged area. Do not apply ice directly to the skin. Put a cloth between your skin and the ice. In the first few days, not apply heat to the area. (How to make an ice bag.)
• Ask your surgical team what type of suture was used to close your wounds. If absorbable sutures were used, they will dissolve with time, and do not need to be removed. Otherwise, sutures are removed around 10 to 14 days after surgery.
• Diet: start with clear liquids and soups following surgery and slowly return to your regular diet. Sometimes the digestive system is slow to respond after anesthesia or while taking narcotic pain medicine and you may become nauseated. Constipation is also a common side effect of narcotic pain medication. Walking around more, taking less narcotic medications, and over the counter laxatives can all help.
• Strong pain pills (narcotics) may be prescribed for the first few days. Pain medicine should be taken exactly as your surgeon prescribes and as needed. Don’t wait to take your pain medicine until you are in a lot of pain; pain medicine works best if you stay ahead of the pain. Do not drink alcohol or drive while taking narcotic pain medication.
• You can take anti-inflammatory medicines along with the pain medicine – but check with your surgical team first. Take all pain medicines with food to prevent an upset stomach. Call your surgeon if you have pain that is not controlled with your pain medicine.
• You can usually remove the surgical bandage in about three days. However, the instructions of your surgeon should always be followed first. Because so much fluid is pumped into your shoulder during the procedure, it is normal for your dressing to have some drainage on it. If the drainage is excessive i.e. you are soaking through numerous dressings, call your surgical team.
• You can take a shower after the bandage is removed in about 3 days. Do not scrub or soak the wound for at least 2 weeks or as directed by your surgical team.
• Though physical therapy is usually started after one to two weeks after the surgery, sometimes simple exercises are given to the patients to do at home just after the surgery as this helps to keep the shoulder joint from getting too stiff.
• Do not drive until your surgeon say it’s okay
• If your job does not require to use the affected arm, you can expect to return to work within three to five days. However, if you heavily depend on your affected arm for work, expect to have to miss work or go on limited duty.
When to Call Your Surgeon or Go to the Nearest Emergency Room
• If you have difficulty breathing.
• If you have swelling or pain in your thigh or calf.
• If the arm you had surgery on changes color or temperature.
• If you have progressive numbness in the affected arm.
• If the pain in the affected arm gets worse even with proper use of pain medication; or if you cannot control the pain with the pain medicine.
* If you have a fever higher than 101.5°F.
• If you have excessive nausea and/or vomiting from the pain medication.
• If you have continuous draining or bleeding from the incisions.
What You Can Expect After Shoulder Arthroscopy
Shoulder arthroscopy is often a better alternative to open surgery in the right situation. Arthroscopy surgery is typically done outpatient — meaning you go home the same day as surgery.
Depending on the surgery that was performed, therapy may be delayed to allow your shoulder to heal first. However, physical or occupational therapy usually end up being a part of the recovery process. They help you to regain shoulder motion and strength. Complete recovery can take as long as 6 months to a year depending on what type of surgery was done.
It is very important to listen to your surgeon’s post-operative restrictions and instructions to ensure maximal recovery. It is a common saying amongst surgeons that “the surgery itself is the easy part of the recovery process.” The result of your surgery depends heavily on you!
