Osteoarthritis is a chronic, degenerative disorder that is defined as the gradual deterioration (or degeneration) of the articular (or hyaline) cartilage in a joint. This noninflammatory disorder may be inherited, follow a trauma, or even be a complication of malformations at birth. It is also related to advanced age.
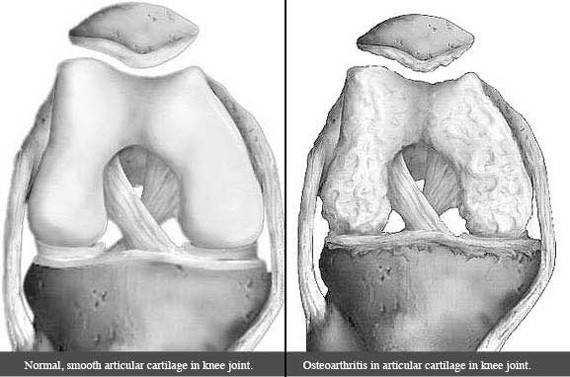
Healthy cartilage is normally smooth and prevents friction when the joint surfaces rub against one another. This allows for smooth, pain-free motion of the joint. Hyaline cartilage additionally serves as a cushion and shock absorber to the underlying bone when there is physical movement.
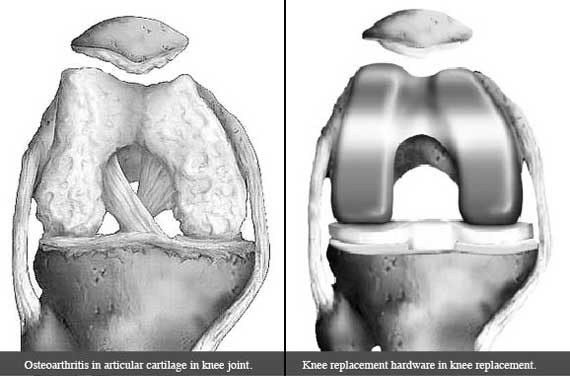
In osteoarthritis, the smooth cartilage of the involved joint wears down, leaving the underlying bone exposed. The surface of exposed bone is typically rough like sandpaper and has a lot of nerve endings. Without their protective cartilage layers, the exposed bones rub together, causing pain, swelling, and loss of motion of the joint.
To better understand osteoarthritis, we should first review healthy joint anatomy.
Healthy Joint Anatomy
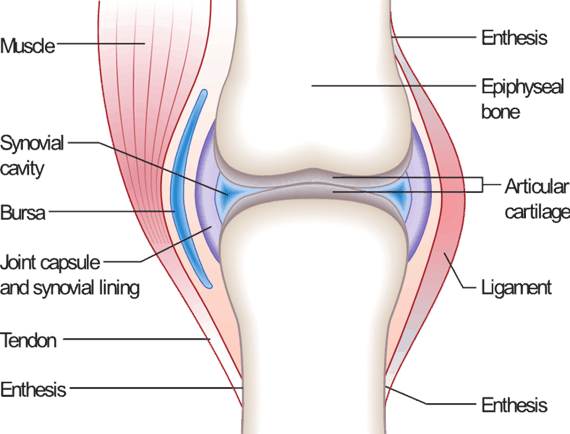
In a healthy joint, the ends of the bones are covered with articular (or hyaline) cartilage. Hyaline cartilage functions as a protective cushion to the underlying bone and a slick surface that enables pain-free and smooth motion at the joint.
Synovial joints are typically surrounded by a tough, fibrous, capsule of connective tissue that connects the bones to one another granting some stability to the joint. Additionally, many of these joints may further be reinforced by additional ligamentous structures e.g. collateral ligaments of the knee.
The joint capsule is lined with a soft tissue structure called the synovial membrane. The synovial membrane (or synovium) consists of cells that produce a slick, lubricating fluid called synovial fluid. Synovial fluid further increases the slickness of the joint surfaces, allowing for very smooth and pain-free motion at the joint.
What Happens in Osteoarthritis?
Osteoarthritis occurs commonly in weight-bearing joints — i.e. mainly in the lower extremity. It can also commonly affect the fingers, wrists, shoulders and spine. In an osteoarthritic joint, the articular cartilage wears down where the bones meet. The surface of exposed bone is typically rough like sandpaper and has a lot of nerve endings. Thus, without its protective cartilage layer, the bones rub against each other causing pain and swelling.
As osteoarthritis progresses, bony outgrowths called osteophytes or bone spurs, appear on the edges of the bone. Synovial fluid is overproduced. As a result of all of this, the joint eventually may become increasingly stiff.
Osteoarthritis mainly affects the elderly and is more common in women. Infection, trauma, developmental disorders, and endocrine disorders, can lead to an earlier onset of arthritis. Additional risk factors include obesity, genetics, and long-term participation in activities that stress joints—e.g. dancing, football, tennis, weightlifting.
Effects of Osteoarthritis
Osteoarthritis does not always cause symptoms for patients. However, it does, joints can become painful and stiff. These symptoms typically worsen with activity and are relieved with rest.
Any of the following joints can be involved:
Fingers and thumb: When affected, the fingers and thumbs can become enlarged. Movement of the joints can be accompanied by pain and stiffness.
Knee: The knee is a commonly affected joint. As arthritis in the knee becomes more severe, it can become very difficult to participate in simple activities of daily living: walking, climbing stairs, etc.
Hips: Similar to the knee, the hip is also commonly affected by osteoarthritis. When symptomatic, the pain can radiate to the groin region, the inner thighs, buttocks, or even to the knees. People affected with hip osteoarthritis often find it difficult to bend or move around.
Spine: Osteoarthritis can also affect the spine. Pain and stiffness in the neck and lower back can be common and if severe, quite debilitating. As osteoarthritis progresses, bone spurs, and other soft tissue structures can begin to pinch on the nerves or even the spinal cord. This can result in numbness and weakness of the arms or legs, depending on structures are being pinched.
Apart from the basic symptoms of joint pain and stiffness, the effects of osteoarthritis differ from person to person depending on the severity of their symptoms. They may find that their symptoms result in:
- Limitations in continuing one’s job
- Limitations in performing activities of daily living
- Depression and anxiety due to chronic pain and disability
Diagnosing Osteoarthritis
Osteoarthritis cannot be diagnosed with one single test. Your doctor will first perform a history and physical examiniation—where you describe your symptoms, that is tell him or her where you hurt. During this appointment, he or she will additionally examine the area of your body that is bothersome.
Depending on what your doctor thinks, he or she may order x-rays to assess the severity of your osteoarthritis. Doctors can use X-rays to get a general sense of the severity of your osteoarthritis. However, in early stages of osteoarthritis, X-rays may appear relatively normal, as not much cartilage is lost in the early stages.
It is important to keep in mind that X-ray evidence of arthritis does not necessarily correlate with your symptoms. i.e. just because you have bad looking joints on X-ray, doesn’t necessarily mean you will have pain or disability or need any treatment.
Certain blood tests may additionally be ordered to rule out other physical ailments which can cause symptoms like osteoarthritis.
Treatment options
The treatment of osteoarthritis involves the following goals:
- Reducing weight or maintaining a normal body weight
- Having a healthy lifestyle
These two lifestyle modifications can help in the other aims of treatment including:
- Controlling pain
- Improving joint mobility and function
Pain Relief Without Medications
There are non-medicinal ways to treat pain associated with osteoarthritis. Here are some examples of this:
Exercise
Exercise is one of the best treatments for osteoarthritis. It is also an inexpensive treatment option. Exercise may help to reduce pain, maintains mobility of the joints, helps with improved weight maintenance, and improves blood flow to the body, which is great for overall health.
Walking, swimming, and water aerobics are good exercises for people with osteoarthritis. A physical therapist can help you find the most appropriate form of exercise. The side effects of exercising are almost zero if the exercises are done properly.
Weight Management
Patients who are overweight or obese are at higher risk of developing osteoarthritis. Weight loss reduces the stress on the affected joints potentially helping to reduce pain in the joint. Consequently, weight reduction should be a top priority both for the prevention and management of osteoarthritis. If needed, a registered dietician or nutritionist can help you with the right weight loss strategies to help achieve a healthy weight.
Other Options
Hot and cold packs – either individually or in combination can additionally be helpful. Hot packs help to increase blood flow to the painful area and decrease pain and stiffness; cold packs help by reducing inflammation and soreness.
Speak with your doctor to choose the right treatment(s) for you.
Medications
There are various pain medications that can be prescribed to help relieve pain and to help patients to carry on with their activities of daily living. Your doctor will take into consideration your previous medical history and other medications the you are already taking. Any of the following are options: acetaminophen (Tylenol), NSAIDs (non-steroidal anti-inflammatory drugs e.g. ibuprofen, naproxen, meloxicam, etc.), tramadol, and topical pain-relieving creams. Most medications have potential side effects, so before taking any medicine, learn as much as you can about any associated allergic reactions.
Beyond medications, injections such as corticosteroids and viscosupplementation may also be an option for the treatment of your pain.
Surgery
It is important to remember that surgery for osteoarthritis is almost always an elective procedure. i.e. You, as the patient, are ultimately the one that must decide that surgery is the next best step for you. This decision usually happens after you have exhausted all non-surgical treatment options and are still experiencing significant pain and debility.
Considering the above, any of the following may then be reasons to consider surgery:
- If loose pieces of bone or cartilage need to be removed because they are causing symptoms of locking or catching of the joint or significant pain. In these situations, knee arthroscopy may be an option for you.
- If pain and debility continue to be quite severe despite non-surgical treatment options, joint replacement surgeries are a very effective option.
See: Hip, knee, and shoulder, anatomy to better understand how osteoarthritis can affect joints.
Many factors like the intensity of pain, level of disability, patient’s age, and patient’s occupation are considered before having surgery. Following surgery, you will work with your physical therapist to get you back to “normal”. See recovery time for shoulder replacement surgery, knee replacement and hip replacement.
Alternative therapies
When the usual treatment options fail to provide pain relief, prior to considering surgery, some people try alternative therapies like acupuncture, nutritional supplementation (glucosamine, chondroitin sulfate, etc.), as well as home herbal remedies. While these treatments have minimal side effects, their benefits have yet to be proven.
What Doctors are involved in the Treatment of Osteoarthritis?
There are several types of doctors that may be involved in the care of your osteoarthritis:
- Primary care physician: Performs initial work-up and may initiate treatment of osteoarthritis. May then refer to other specialists if needed.
- Rheumatologist: Specializes in the medical care of patients with diseases that affect the musculoskeletal system.
- Orthopedic Surgeon: Specializes in both the non-surgical and surgical treatments of bone and joint diseases
What You Can Do To Manage your Osteoarthritis
The following tips can help you control your symptoms and enjoy better health:
- Learn as much about osteoarthritis as you can. A good understanding of osteoarthritis will help you deal with it better. Consider enrolling in an arthritis support group or self-management program.
- Have an active lifestyle. Exercise regularly. Include strengthening exercises, aerobics, and range-of-motion exercises to reduce stiffness and maintain your overall strength and fitness. Always talk with your doctor before starting any form of exercise. Your doctor can tell you which exercises will be the best for your situation.
- Eating a balanced diet can help you to keep fit. Try to eat a diet that will help you lose or maintain a healthy weight. Added weight puts pressure on your affected joints. This causes more discomfort and pain.
- Most importantly, keeping a positive attitude can affect your physical health. Participate in fun activities like sports or other hobbies.
Note that the information in this article is purely informative and should never be used in place of the advice of your treating physicians.