If you get the chance to help prepare your partner or friend by coaching them through labor, these tips will help you be a great coach.
Labor Vocabulary
- Active Labor
- stage of labor where the cervix is between 4 to 7 cms. Contractions are
2-4 minutes apart lasting 60 seconds or longer. - Amniotic Sac
- ‘bag of waters’; fluid surrounding the baby that protects him against injury and infection.
- Bloody Show
- pink to bright red vaginal discharge that occurs as the cervix thins and opens during labor.
- Braxton-Hicks
- intermittent contractions of the uterus present throughout pregnancy but more noticeable in the last trimester. Sometimes call “false labor” as it does not cause the cervix to open.
- Cervix
- mouth of uterus; thins out (effacement) and opens up (dilation) during labor.
- Dilatation
- gradual opening of cervix during labor. Usually measured in centimeters with 10 centimeters meaning completely dilated.
- Early Labor
- stage of labor where cervix is between 1-3 cms and contractions are 5-20 minutes apart lasting 30-45 seconds. This is the longest phase of labor.
- Effacement
- gradual thinning and shortening of the cervix. Measured in percentage – 100% is totally effaced.
- Fundus
- top of uterus; grows upward during pregnancy; the fundus is measured for size at each prenatal visit.
- Lightening
- process where baby settles into the pelvis. Commonly referred to as the baby “dropping”; clothes fit differently all of a sudden breathing may be easier.
- Mucus Plug
- a slightly pinkish-white mucous substance which has kept the uterus sealed during pregnancy. It is a sign that your cervix is “ripe” and labor may be starting within a couple of days.
- Pelvic Bones
- ring of bones around uterus that baby passes through during labor.
- Pelvic Floor Muscles
- group of muscles that form a figure 8 to support bladder, rectum and vagina. Important to exercise these muscles and to keep the muscles strong.
- Placenta
- attached to uterus; transfers food, oxygen and anything else mother takes into baby; comes out “after birth” of baby.
- Pushing
- stage of labor where cervix is completely dilated. Pushing is done with contractions to help the baby’s passage through the birth canal.
- Rupture of Membranes
- where the amniotic sac breaks, allowing the amniotic fluid to leak out of the uterus. If this happens at home, tell your doctor.
- Station
- a measurement of descent of the baby’s head through the pelvis.
- Transition
- shortest phase of labor as well as the most intense part of labor. Cervix is between 7-10 cms with contractions 2 minutes apart lasting 90-120 seconds. These contractions are intended to finish dilating the cervix.
- Umbilical Cord
- connects baby to placenta; about 40 inches long, with blood pumping through it; baby’s lifeline.
- Uterus
- womb; muscle that holds baby during pregnancy; non-pregnant is about the size and shape of a pear.
- Vagina
- elastic like canal that serves as a passage from outside body to inside — also called birth canal.
The uterus is a large muscle. Like other muscles, it can tighten and contract. When it is time for birth, a hormone is released that causes the uterus to begin regular contractions, called labor. Labor contractions are not voluntary. Therefore, you cannot control how long they last, how often they happen, or how strongly they contract.
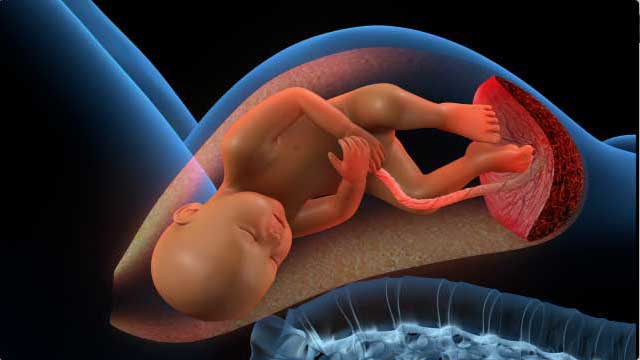
Contractions in the uterus push the baby out. When the uterus contracts, you should be able to feel the tightness with your fingertips. The whole surface of your uterus will feel hard, not just one area like a foot or your baby’s rump. A contraction has three phases: the build up, the peak, and the letting down. That is, each contraction gets stronger up to a peak, and then gradually eases off. During a contraction, your uterus may seem to tighten into hard ball, then relax and soften.
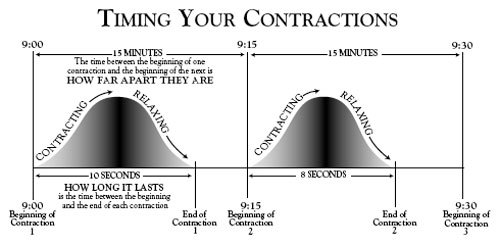
Once you have a contraction, you should begin monitoring them, even if it is only a single contraction. Be sure to write down the time, date, and the timing of your contractions. The timing of your contractions is the frequency and duration of each contraction. The frequency is how much time passes (“minutes apart”) between the beginning of one contraction and the beginning of the next contraction. Duration is how long the contraction last. For example, assume a contraction lasts for 1 minute (the duration), and then it is 4 minutes until the next contraction (the interval). The frequency is the duration plus the interval, or 5 minutes. It is important to know the frequency because your doctor or certified nurse midwife may tell you to go to the hospital when your contractions are “so many” minutes apart.
As labor progresses, the time between contractions gets shorter, the duration gets longer, and the intensity increases. During early labor, the duration is about 30 seconds. As labor continues the duration increases to about 45 to 90 seconds. Also, as labor progresses, the frequency increases to one contraction every 2 to 3 minutes.
Once labor begins, call your doctor or certified nurse midwife if you feel dizzy or lightheaded, have a persistent headache or a fever, your vision is blurry, or you think something is wrong. You should also call your doctor or certified nurse midwife if you begin having more than 4 contractions per hour before your 37th week.
Early Labor
~ Rest; stay calm
~ Shower (if bag of waters has not broken)
~ Time contractions
~ Early breathing pattern (regular, easy breaths throughout contraction)
~ Call MD or NM when contractions have regular pattern
~ Drink clear liquids only
~ Walk
Active Labor
Comfort Suggestions
~ Change positions as often as necessary. Try:
• Sitting
• Reclining backwards (not flat)
• Lying on either side
• Leaning forward over a stack of pillows
• On all fours (especially for back labor)
• Leaning on support person
• Massage
~ Urinate often
~ Cool or warm washcloth
~ Ice chips after breathing with a contraction
~ Lip Balm
~ Touch – soft gentle massage
~ Breathing patterns should be slow, controlled and relaxed, enough for comfort and to save energy.
~ Medicine – mother’s decisions for medicine have nothing to do with success or failure – mother’s comfort level is important.
~ Apply counterpressure to lower back using tennis ball, your hands, or a rolled up towel for back support.
~ Relax between contractions – let go… trust the body to deliver your baby
~ Work with the contractions rather than fighting them.
Transition
~ Coach should not leave at this time
~ Contractions are stronger and longer
~ Breathing is at a rate to keep up comfort (pant-blow)
~ Fastest stage of labor
~ Offer words of encouragement:
• “I love you.”
• “Good job.”
• “I’m proud of you.”
• “The contraction has peaked.”
• “We’re making progress.
~ Maintain calmness, confidence, and patience
~ Breathe with the mother (pant-blow)
~ Encourage the mother’s feeling of control
~ May have “mood swings”
~ Change positions as often as necessary. (See above Comfort Suggestions.)
~ Try not to push until advised to by your certified nurse midwife, or doctor.
Pushing During Labor
~ Requires lots of energy
~ Push only when cervix is fully dilated
~ Hands on lower thigh behind knee for support and traction
~ Chin on chest
~ Rest between contractions
~ May want to change positions
• “C” position
• On all fours (especially for back labor)
• side-lying – coach holding leg
~ Long, hard pushes are most effective. Deep breath and push down for a count of 10 if possible, repeat pattern through contraction. Assist the laboring mother when she is discouraged about her progress by reminding her:
~ of the progress she has made
~ that many women get discouraged
~ of relaxation techniques, paced breathing and other coping skills
~ of the need to take each contraction, one at a time, rather than focusing on remaining labor.
You can give her
~ Attention — lots of it!
~ Support — both verbal and physical
~ Confidence — by remaining calm and communicating to her that she can cope effectively.
When the going gets tough
If the laboring mother feels a desire to give up, is no longer using breathing pattern effectively, or expresses the need for help, you can:
~ Use eye-to-eye contact; without using words this says “I am here and I can help”
~ Hold her hand firmly and say “I can help, I know what to do.”
~ Get her total attention by placing your face within 10 inches of her face.
Breathe with her, use your eyes as her focal point.
~ Use your hands to turn her face toward yours. Breathe with her until she refocuses on her breath. When her breathing rate has slowed, change to a paced breathing pattern to lead her back into controlled breathing. Move your head in a nodding motion and stroke down her arms with each exhalation.