Achilles tendonitis refers to inflammation or irritation of the connective tissue band that attaches the calf muscle to the heel. It occurs as a result of factors that put excessive stress on the Achilles. A sudden increase in exercise intensity or frequency is a common cause. Chronic overuse can create micro-tears within this tendon, leading to weakening or “wear and tear” over time. This can cause thickening of the tendon, and the formation of scar tissue.
Learn All About the Anatomy of Feet and Ankles and Common Problems
If treated promptly, many cases of Achilles tendonitis are short-lived. Prolonged tendonitis, however, can cause persistent pain and disability. Scar tissue may form during the healing process which limits the flexibility of the tendon, and increases the likelihood of a rupture.
Fortunately, most cases resolve with rest and over-the-counter medications. For others, calf muscle exercise therapy or other treatments may be needed. Ignoring the symptoms can result in a rupture or tear of the tendon which would require surgery.
Before you read any further, it might help to brush up on Foot and Ankle Anatomy.
Where is the Achilles Tendon and What Does it Do?
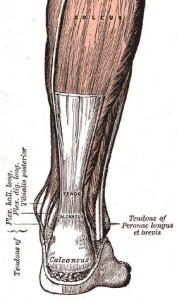 Tendons are strong, fibrous connective tissues that attach muscles to bones. As muscles contract, they pull on the tendon to move the attached body part. The achilles tendon connects two calf muscles, the outer gastrocnemius and the underlying soleus, to the back of the heel (calcaneus bone).
Tendons are strong, fibrous connective tissues that attach muscles to bones. As muscles contract, they pull on the tendon to move the attached body part. The achilles tendon connects two calf muscles, the outer gastrocnemius and the underlying soleus, to the back of the heel (calcaneus bone).
When contracted, the calf muscles pull the achilles tendon upward, causing the foot to point downward. This allows you to stand on your toes. When relaxed, it lowers your heel to the ground. This powerful calf muscle group helps you to sprint, jump, or climb. It provides the “push-off phase” of walking and running.
What Causes Achilles Tendonitis?
The achilles tendon is one of the strongest in the body, but is prone to injury because of the tremendous pressure that it endures with every step we take. Achilles tendonitis is often an overuse injury, meaning doing too much too soon.
Problems with the Achilles tendon most often affect athletes, especially runners, basketball players, and participants of sports that require jumping (i.e. volleyball, tennis). Age is also a factor, and this type of tendonitis is common among middle-aged adults. Tendonitis can also occur when calf muscles become too tight over time, or because of how they developed prior to birth. Injuries can be minor or rather severe.
Achilles tendonitis may be acute, developing a few days after an increase in exercise training, or become a chronic issue. For example, it follow a sudden increase in running, especially if a greater distance, speed, or hilly terrain. Risk factors for non-athletes include diabetes, gender (more common in men), obesity, steroid medications or recreational use, and certain antibiotics. Individuals who only engage in intense exercise on weekends are also at risk.
What do Achilles Tendon Problems Feel Like?
Acute:
- Gradual onset of pain on the back of the leg or ankle over a period of days
- Pain at the onset of exercise that improves with continued exercise
- Pain gets better with rest
- Tenderness with pressure on the affected area
Chronic Achilles tendonitis can develop when acute tendonitis is left untreated. This type is more difficult to manage.
- Gradual onset of pain that lasts weeks to months
- Pain that is constant throughout exercise
- Pain while walking uphill or up stairs
- Pain and stiffness in the tendon after a period of rest, especially early in the morning
- Nodules or lumps within the tendon
- Tenderness of the tendon with pressure
- Swelling or thickening of the tendon
- Skin redness over the affected area
- A “creaking” sensation when moving the ankle or pressing the tendon with your fingers
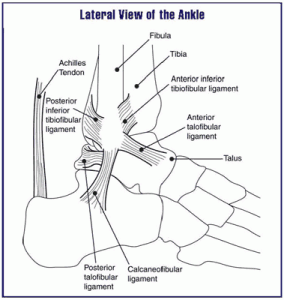 There may be pain at the point where the Achilles tendon attaches the calcaneus. Here, a fluid-filled sac lies between the tendon and the bone, called a bursa. It limits friction as the tendon glides up and down at the back of the heel bone. When this sac becomes inflamed, it is called bursitis. This condition is characterized by pain and irritation at the back of the heel. You may notice redness or swelling. Shoes can aggravate bursitis, making it difficult to wear enclosed shoes. Some shoes are better than others for this issue.
There may be pain at the point where the Achilles tendon attaches the calcaneus. Here, a fluid-filled sac lies between the tendon and the bone, called a bursa. It limits friction as the tendon glides up and down at the back of the heel bone. When this sac becomes inflamed, it is called bursitis. This condition is characterized by pain and irritation at the back of the heel. You may notice redness or swelling. Shoes can aggravate bursitis, making it difficult to wear enclosed shoes. Some shoes are better than others for this issue.
 Tendonitis refers to the portion of the tendon that is just above the heel. It can become strained where the calf muscles attach the Achilles tendon, or along the length of the tendon itself. There may be pain when it is pressed, and with walking or motions that require putting weight on your toes such as going down stairs or stepping off a curb. (See xray image left.)
Tendonitis refers to the portion of the tendon that is just above the heel. It can become strained where the calf muscles attach the Achilles tendon, or along the length of the tendon itself. There may be pain when it is pressed, and with walking or motions that require putting weight on your toes such as going down stairs or stepping off a curb. (See xray image left.)
How are Achilles tendon problems identified?
Your doctor will make the diagnosis by first taking a history, asking “what were you doing when the pain started?” He or she will examine your calf, ankle, and foot to locate areas of pain or discomfort. Depending on the findings, imaging studies may be recommended. An x-ray can detect fractures, heel spurs, or other bone problems. An ultrasound can assess the amount of tendon injury.
What Are My Treatment Options?
Treatment options will depend on the severity of your injury, and how long it has been since it occurred. First-line management is typically rest, ice, and anti-inflammatory medicines such as NSAIDs.
- Rest:
- Resting the painful Achilles tendon allows the inflammation to subside to promote healing. A period of rest includes stopping the activity that is causing the pain. This prevents further damage to the tendon.
- Immobilization:
- For patients who have more significant symptoms, a period of immobilization can help. Either a removable walking boot, or sometimes even a cast, can quickly reduce the amount of inflammation. Wearing a walking boot prevents the calf muscle from pulling on the Achilles tendon, thus relieving strain on it. It also prevents you from pushing off with the ball of your foot, or pointing your toes downward. This device should primarily be worn when walking. However, there is some benefit to wearing the boot even at rest as it maintains a slight stretch on the Achilles tendon, and prevents further shortening.
- Night Splint:
- A night splint keeps the foot in a similar position as the walking boot with a gentle stretch on the Achilles tendon. However, it is not sturdy enough to use for walking.
- Daily use of a night splint while sedentary, from minutes to several hours, can improve the outcome of physical therapy by continuing the rehabilitation at home. After recovery, a night splint can help prevent recurrent strains, and maintains lower extremity flexibility, especially among athletes.
Physical Therapy for Achilles Tendonitis
For some injuries, physical therapy is recommended to help reduce the formation of scar tissue, and to control pain and swelling. Patients with mild symptoms of bursitis or tendonitis often do well with two to four weeks of physical therapy.
The physical therapist’s goal is to keep the pain and swelling under control, improve your range of motion and strength, and make sure you regain a normal walking pattern. Treatments such as ultrasound, moist heat, and massage are used to control pain and inflammation. As the pain eases, treatment progresses to include stretching and strengthening exercises.
Physical therapy can also include ice. The key to proper ice and heat therapy is knowing when to ice and heat an injury. Your physical therapist knows when and how to apply such treatments to reduce swelling and pain while fostering the healing process. He or she may teach you a home-care program to go along with the in-office treatments.
One purpose of treatment is to break up scar tissue that has formed, stretching it to help the tendon return to normal flexibility without tearing or causing pain. Injured tendons shorten and must be stretched in order to regain normal function.
It is important to follow the instructions of the physical therapist, and be careful to not overdo the stretching. Only gentle stretches for the calf muscles and Achilles tendon are indicated at first. As the tendon heals and pain resolves, more aggressive stretches can be done. If unsure, ask your therapist, “On a scale of one to 10, how much should I be stretching the tendon.” To prevent further scar tissue formation, ice is applied after stretching, massage, or treatments. Doing too much too soon can slow down the healing process by adding further injury to the tendon.
- Ultrasound
- Ultrasound, using high or low frequency sound waves, increases blood flow into the tendon. This prevents the formation of scar tissue, and reduces swelling. The vibrating sound waves can travel deep into the calf muscles and Achilles tendon, creating gentle heat. This heat helps the blood flow to deliver oxygen and nutrients, and remove cellular wastes. The deep heat also helps relieve pain, inflammation, and muscle spasms. Ultrasound is painless. You may feel a mild tingling or nothing at all.
- Electrical Stimulation
- Low-energy shock wave therapy has been used successfully for chronic tendonitis. No anesthesia is required, and it is done over several treatment sessions. The vibrations produced by the energy waves are applied to any areas of pain. In this way, shock wave therapy stimulates soft-tissue healing by increasing blood supply to the treated area.
- Small electrode pads are placed over the painful area while the therapist controls the degree of “shock” to the area. Treatments can last as long as 20 minutes. During the treatment, the intensity of the waves can be adjusted as needed. You may feel a tingling sensation, but no pain.
Electrical stimulation can also be used in conjunction with iontophoresis. This treatment involves the application of a topical anti-inflammatory medication to the treatment area. In theory, the electrical stimulation allows the medication to penetrate the tissues better.
- Steroid Injections
- Steroid injections are rarely used because it is believed they can weaken the tendon, increasing the risk of a tendon rupture.
What to Expect After Treatment
Mild symptoms should respond well to treatment within two to four weeks. More severe injuries can take as long as two to three months to resolve. As your condition improves, calf muscle strengthening exercises can be resumed per the recommendations of your physical therapist. Strengthening starts gradually, using exercises that work the calf muscles, but protect the healing area.
Eventually, you can do specialized strengthening exercises that work the calf muscle while the Achilles tendon lengthens. For example, standing on your tiptoes, then carefully lowering your heels back to the ground.
When your healing is well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of your ongoing home exercise program. At this point, you may be should be able to resume normal activities. If you are an athlete, rehabilitation will be customized for your sport.
It is important to properly rehabilitate the Achilles tendon after you recover from the injury to prevent further issues.
Questions About Achilles Tendonitis
• Q. How long do you have to wear walking boot?
A. The length of time a walking boot is needed depends on the severity of your injury. Your first follow-up visit will likely be two weeks after the boot is prescribed. If there are other factors that could affect your progress, it may be recommended that you wear the boot for a month before the follow-up appointment. If there is no improvement after two weeks, physical therapy is the next step which may include massage and stretching exercises. The main goal of wearing the boot is to rest the tendon.
The downside of this device is that you can lose muscle tone in your foot and calf from lack of use. The boot should be removed at night during sleep. Achilles tendonitis can be caused by calf muscle inflexibility. Even while sitting, wearing the boot will position your foot in a way that slightly stretches your calf muscles. Your doctor or PT may also prescribe a night boot for you to sleep in. The night boot is softer than the walking boot, and is designed to keep a constant, slight stretch on your calf muscles. Because of the poor blood supply in this area, Achilles tendonitis can heal very slowly.
Without proper treatment, further injury of the Achilles tendon may require surgery which may be curative or result in other complications.